A Revolution in Wound Care: Exploring the Latest in Healing Technology
Slow-healing wounds pose significant challenges. This listicle examines eight innovative wound healing technology solutions designed to improve healing outcomes and reduce recovery time. Discover how rapid wound care, negative pressure wound therapy, advanced dressings, bioengineered skin, electrical stimulation, hyperbaric oxygen, ultrasound, and smart monitoring systems are transforming wound care in 2025. This information empowers patients and healthcare providers alike to make informed decisions about the best treatment options.
1. Rapid Wound Care
Rapid Wound Care stands out as a leading wound healing technology solution, bringing expert wound care directly to patients in the comfort of their homes or long-term care facilities. This approach is especially beneficial for individuals dealing with chronic wounds, pressure injuries, diabetic ulcers, and other complex conditions that require consistent and specialized attention. Their team of certified professionals utilizes advanced wound healing technologies, including debridement, advanced dressing applications, infection control techniques, and negative pressure wound therapy, all designed to accelerate the healing process and improve patient well-being. By focusing on a rapid response time, often engaging with patients within 24 hours of referral, Rapid Wound Care significantly reduces the need for costly and often stressful emergency room visits. This proactive approach ensures patients receive continuous, tailored treatment, effectively bridging the gap between healthcare providers and patients in need.
One of the key advantages of Rapid Wound Care is its comprehensive and personalized approach. Treatment plans are tailored to each patient’s unique wound and overall health needs, optimizing outcomes. This personalized approach, combined with the use of cutting-edge wound healing technology like negative pressure wound therapy, significantly contributes to faster and more effective healing. The convenience of at-home or in-facility care enhances patient comfort and accessibility, removing the burden of frequent travel for treatments. Furthermore, the service is designed to be insurance-friendly, with support from Medicare Part B and other insurance programs, simplifying referrals and appointments. Learn more about Rapid Wound Care to explore their extensive service offerings.
Pros:
- Rapid Response: Initiates care within 24 hours, minimizing complications and preventing unnecessary ER visits.
- Personalized Treatment: Tailored plans address individual wound and health needs.
- Advanced Therapies: Employs innovative techniques, including negative pressure wound therapy and professional debridement.
- Convenient Access: Provides care at home or in long-term care facilities.
- Insurance Coverage: Supported by Medicare Part B and other insurance providers.
Cons:
- Limited Availability: Service access may depend on geographic location and insurance coverage.
- Care Coordination: May require coordination with existing primary care physicians or wound specialists for optimal care continuity.
While pricing information is not readily available, the accessibility through insurance coverage makes Rapid Wound Care a viable option for many patients. Technical requirements are minimal, primarily focusing on access to a phone for initial consultations and scheduling. Compared to traditional wound care, which often involves multiple appointments at different locations, Rapid Wound Care offers a more streamlined and patient-centered experience. For patients, families, and healthcare providers seeking efficient and advanced wound healing technology, Rapid Wound Care represents a significant step forward in improving the quality of life for those living with chronic or acute wounds. This service's dedication to personalized, accessible, and technologically advanced care justifies its prominent position on this list.
2. Negative Pressure Wound Therapy (NPWT) Systems
Negative Pressure Wound Therapy (NPWT) systems represent a significant advancement in wound healing technology, offering a powerful tool for managing a variety of complex wound challenges. This therapy utilizes a vacuum mechanism to create negative pressure at the wound site, effectively jumpstarting the healing process. It deserves its place on this list due to its proven efficacy in accelerating healing for chronic, acute, and post-surgical wounds, ultimately improving patient outcomes. Learn more about Negative Pressure Wound Therapy (NPWT) Systems
NPWT works by removing excess fluid (exudate) and reducing edema (swelling), which can impede healing. By drawing out these fluids, the therapy also helps decrease bacterial colonization in the wound bed, minimizing the risk of infection. Furthermore, NPWT promotes increased blood flow to the wound area, which delivers essential nutrients and oxygen needed for tissue regeneration and granulation tissue formation.
Leading NPWT systems, such as the V.A.C. (KCI) Therapy system (https://www.kci-medical.com/us-eng/vac-therapy), utilize specialized dressings (foam or gauze) that are placed directly on the wound bed and sealed with an airtight film. A connected vacuum pump then creates negative pressure (typically -125 mmHg) within the sealed dressing, drawing out fluid and promoting healing. The fluid is collected in a canister attached to the system.
Key Features and Benefits:
- Adjustable Pressure Settings: NPWT systems offer continuous or intermittent negative pressure application, allowing clinicians to tailor the therapy to the specific needs of each wound and patient.
- Specialized Dressings: The use of specialized foam or gauze dressings ensures even distribution of negative pressure across the wound bed, maximizing effectiveness.
- Portability: Many NPWT units are portable, allowing patients greater mobility during treatment and improving their quality of life.
- Digital Monitoring: Modern systems incorporate digital monitoring capabilities to track therapy parameters (pressure, duration, etc.) and alert healthcare providers of any potential issues, ensuring optimal treatment delivery.
- Multiple Therapy Modes: Advanced NPWT systems offer various therapy modes to address different wound types and stages of healing.
Practical Applications and Use Cases:
NPWT is particularly beneficial for treating chronic wounds like diabetic foot ulcers, pressure ulcers, and venous leg ulcers. It is also effective in managing acute wounds such as traumatic injuries, dehisced surgical wounds, and burns. In post-surgical settings, NPWT can help reduce the risk of surgical site infections and promote faster closure of incisions.
Implementation and Setup Tips:
Proper training is crucial for healthcare professionals utilizing NPWT. This includes understanding the different dressing types, pressure settings, and contraindications for the therapy. Clinicians should also be proficient in assessing wound characteristics and selecting the appropriate NPWT mode for optimal results.
Pros and Cons:
Pros:
- Effectively reduces edema and removes excess exudate.
- Decreases bacterial colonization and infection risk.
- Promotes faster granulation tissue formation and wound closure.
- Reduces nursing time for dressing changes compared to traditional wound care.
Cons:
- Higher initial cost compared to traditional wound care (approximately $100-200 per day).
- Potential for pain during therapy and dressing changes, which can be managed with appropriate pain management strategies.
- Contraindicated for certain wound types, such as untreated osteomyelitis, necrotic tissue with eschar, and malignancy in the wound bed.
- Requires specialized training for proper application and monitoring.
This advanced wound healing technology offers a powerful solution for complex wound management. While the initial cost may be higher than traditional methods, the potential benefits of accelerated healing, reduced infection rates, and improved patient outcomes often outweigh the expenses, making NPWT a valuable tool in modern wound care.
3. Advanced Wound Dressings with Growth Factors
Chronic wounds, such as diabetic foot ulcers, present a significant challenge in healthcare, often resisting traditional treatment methods and impacting patients' quality of life. Advanced wound dressings with growth factors represent a significant advancement in wound healing technology, offering a targeted approach to accelerate the healing process. These dressings incorporate bioactive proteins that mimic the body's natural signaling molecules, stimulating cell growth, blood vessel formation (angiogenesis), and the production of extracellular matrix – the structural framework for tissue repair. This active intervention helps jumpstart the healing cascade in wounds where normal processes are compromised. One example is Regranex Gel (becaplermin), which delivers platelet-derived growth factor-BB (PDGF-BB) directly to the wound site. Learn more about Advanced Wound Dressings with Growth Factors
These advanced dressings are available in various formats, including gels, sheets, and sprays, catering to different wound types and locations. Many incorporate controlled-release delivery systems, ensuring a sustained therapeutic effect over time. Biocompatible carrier materials help maintain a moist wound environment, crucial for optimal healing. Some formulations even combine growth factors with antimicrobial components to address infection risk, a common complication in chronic wounds. This multifaceted approach makes these dressings a valuable tool in managing complex wound cases.
Features and Benefits:
- Targeted Therapy: Recombinant human growth factors specifically target the molecular pathways impaired in chronic wounds, addressing the root cause of delayed healing.
- Sustained Release: Controlled delivery systems ensure consistent growth factor concentration at the wound site, maximizing therapeutic efficacy.
- Moist Wound Healing: Biocompatible carriers promote a moist environment conducive to cell migration and tissue regeneration.
- Infection Control: Some dressings include antimicrobial agents to prevent and manage wound infections.
- Various Applications: Available in diverse formats (gels, sheets, sprays) to accommodate different wound types and patient needs. Some formulations are suitable for at-home application, empowering patients in their own care.
Pros:
- Effective in stimulating healing in stalled or chronic wounds resistant to standard care.
- Generally well-tolerated with minimal side effects.
- Can reduce healing time and improve overall patient outcomes.
- Some products offer convenient at-home application.
Cons:
- High Cost: These advanced dressings can be expensive. Regranex, for example, costs approximately $1,200 per 15g tube, which can pose a financial barrier for some patients. Medicare and insurance coverage varies and should be investigated.
- Consistent Application: Requires regular and consistent application to maintain the therapeutic effect.
- Variable Effectiveness: Treatment outcomes can vary depending on individual patient factors, wound characteristics, and adherence to the treatment regimen.
- Potential Cancer Risk: Some growth factor products carry FDA warnings about a potential increased risk of cancer with long-term use. This risk should be carefully discussed with a healthcare professional.
Website: Smith & Nephew Advanced Wound Management
These advanced dressings with growth factors deserve a prominent place in the wound healing technology landscape because they offer a targeted, biologically driven approach to address the complex challenges of chronic wounds. While cost and potential risks are important considerations, the potential benefits of accelerated healing and improved patient outcomes make these dressings a valuable tool for healthcare providers specializing in wound care. Patients and caregivers should consult with their medical team to determine if growth factor therapy is appropriate for their specific wound and health situation.
4. Bioengineered Skin Substitutes: A Breakthrough in Wound Healing Technology
Bioengineered skin substitutes represent a significant advancement in wound healing technology, offering a viable solution for complex and challenging wounds that may not respond to traditional treatments. These innovative products are designed to mimic the natural structure and function of human skin, providing a temporary or permanent covering that actively promotes tissue regeneration. This makes them a crucial tool for patients with chronic or acute wound conditions, primary care providers, long-term care facilities, wound care specialists, and even Medicare and insurance beneficiaries grappling with the cost of complex wound care.
These substitutes are created using advanced tissue engineering techniques, combining a structural matrix (often made of animal collagen or synthetic materials) with living cellular components, such as human cells. Products like Integra and Apligraf exemplify this technology, offering different compositions and functionalities tailored to specific wound types. Some even incorporate multiple layers representing both the epidermis (outer layer) and dermis (inner layer) of the skin, further replicating the natural skin architecture. This intricate design allows the substitute to integrate with the patient's own tissue, stimulating cell migration, vascularization (new blood vessel growth), and ultimately, faster wound closure.
Practical Applications and Use Cases:
Bioengineered skin substitutes are particularly valuable in treating a range of complex wounds, including:
- Chronic ulcers: Such as diabetic foot ulcers, venous leg ulcers, and pressure ulcers, which often struggle to heal naturally.
- Burns: Both partial and full-thickness burns can benefit from the immediate wound coverage and reduced infection risk offered by these substitutes.
- Surgical wounds: Especially large or complex surgical wounds where traditional closure methods might be insufficient.
- Traumatic injuries: Skin substitutes can aid in the reconstruction of skin lost due to trauma.
Features and Benefits:
The power of bioengineered skin substitutes lies in their ability to actively promote healing, rather than passively covering the wound. Key features and benefits include:
- Living cellular components: These components secrete growth factors and cytokines, signaling molecules that orchestrate the healing process and stimulate tissue regeneration.
- Mimics natural ECM: The structural matrix mimics the natural extracellular matrix (ECM), providing a scaffold for cell attachment and migration.
- Variety of sizes: Substitutes are available in various sizes to accommodate different wound dimensions, ensuring optimal coverage.
- Gradual biodegradation: The substitute breaks down gradually as the patient's own tissue regenerates, creating a seamless transition.
Pros and Cons:
While highly effective, bioengineered skin substitutes come with important considerations:
Pros:
- Immediate coverage: Offers rapid coverage for large or complex wounds, minimizing infection risk.
- Enhanced healing: Creates a favorable environment for host cell migration and proliferation, accelerating the healing process.
- Alternative to autografting: Can be a viable option when autografting (taking skin from another part of the patient's body) is not feasible.
Cons:
- High cost: These substitutes are expensive, ranging from $1,500 to $3,000 per application.
- Limited shelf life: Requires specialized storage conditions due to the presence of living cells.
- Potential for rejection: Some products carry a risk of immune rejection, although this is less common with newer generations of substitutes.
- Requires surgical expertise: Proper application necessitates surgical expertise and training.
Implementation and Setup Tips:
Application of bioengineered skin substitutes typically involves preparing the wound bed, carefully positioning the substitute over the wound, and securing it with sutures or dressings. Given the complexity and cost, these procedures are generally performed by trained wound care specialists or surgeons. Patients requiring this treatment should consult with a healthcare professional experienced in advanced wound care techniques.
Why Bioengineered Skin Substitutes Deserve Their Place:
Bioengineered skin substitutes earn their spot on this list due to their unique ability to actively participate in the wound healing process. They go beyond simply covering the wound; they actively promote tissue regeneration, making them a vital tool in the fight against chronic and complex wounds. This innovative wound healing technology offers hope for patients who have exhausted other treatment options and are searching for effective solutions. For more information on Integra's wound reconstruction products, visit https://www.integralife.com/wound-reconstruction.
5. Electrical Stimulation Devices: A Spark for Faster Wound Healing
Electrical stimulation devices represent a cutting-edge approach to wound healing technology, offering a non-pharmaceutical option for accelerating the body's natural healing processes. These devices utilize controlled electrical currents to mimic the body’s bioelectrical system, which plays a vital role in tissue repair. This makes them a valuable tool for patients with chronic or acute wound conditions, primary care providers, long-term care facilities, wound care specialists, and even Medicare and insurance beneficiaries seeking advanced treatment options. Elderly patients, often facing challenges with slower healing, can also benefit from this technology.
Systems like the WoundEL and Provant Therapy deliver various waveforms and current types – including microamperage, pulsed, and direct current – directly to the wound area. This targeted electrical stimulation works on multiple levels to promote healing:
- Stimulates Cell Migration: Encourages the movement of key cells involved in tissue repair to the wound site.
- Increases Protein Synthesis: Boosts the production of essential building blocks for new tissue growth.
- Enhances Blood Flow: Improves circulation to the wound area, delivering oxygen and nutrients necessary for healing.
- Reduces Bacterial Load: Exhibits potential antimicrobial effects, minimizing the risk of infection.
These devices are particularly effective for wounds with compromised circulation or persistent inflammation, conditions often encountered in chronic wounds and the elderly.
Features and Benefits:
Electrical stimulation devices offer a range of features designed for effective and convenient therapy:
- Adjustable Current Parameters: Amplitude, frequency, and waveform can be tailored to individual patient needs and specific wound types, allowing for personalized therapy.
- Non-invasive Electrodes: Applied directly to the wound bed in conjunction with standard wound dressings.
- Programmable Treatment Schedules: Ensures consistent therapy delivery, crucial for optimal healing.
- Portable Designs: Suitable for both home and clinical use, offering flexibility for patients and healthcare providers.
- Digital Interfaces: Enable therapy monitoring, patient compliance tracking, and data-driven adjustments to treatment plans.
Learn more about Electrical Stimulation Devices
Pros and Cons:
While electrical stimulation offers a promising avenue for wound healing, it's important to consider both the advantages and disadvantages:
Pros:
- Non-pharmaceutical: Provides a drug-free alternative for patients seeking to minimize medication use.
- Minimal Side Effects: Generally well-tolerated, with fewer side effects compared to some pharmaceutical interventions.
- Adjunctive Therapy: Can be used in conjunction with other wound care modalities to enhance their effectiveness.
- Accelerated Healing: Shows potential for jumpstarting the healing process in stalled chronic wounds.
- Antimicrobial Effects: May reduce the risk of infection, a critical concern in wound management.
Cons:
- Variable Evidence Base: The level of evidence supporting the efficacy of electrical stimulation varies across different wound types. More research is needed to fully establish its effectiveness for all wound conditions.
- Inconsistent Insurance Coverage: Accessibility can be limited due to variations in insurance coverage and reimbursement policies.
- Requires Training: Effective home use necessitates proper training for patients or caregivers on device operation and application.
- Contraindications: Not suitable for all patients, particularly those with certain implanted electronic devices (pacemakers, defibrillators, etc.).
Implementation and Setup:
Successful implementation involves proper patient assessment, wound evaluation, and selection of appropriate device settings. Healthcare professionals should provide thorough training on electrode placement, device operation, and treatment schedules. Regular monitoring of the wound's response to therapy is crucial for optimizing treatment outcomes.
Pricing and Availability:
Pricing for electrical stimulation devices varies depending on the specific model and features. For instance, the WoundEL Microcurrent Stimulation Device is available at https://www.apothecary-options.com/wound-el-microcurrent-stimulation-device/. Consulting with a wound care specialist or supplier can provide more detailed pricing information and guidance on selecting the appropriate device.
Electrical stimulation devices offer a unique and potentially valuable addition to the arsenal of wound healing technology. By harnessing the power of the body's own bioelectrical system, these devices offer a promising path toward faster, more effective wound healing for a wide range of patients.
6. Hyperbaric Oxygen Therapy (HBOT) Chambers
Hyperbaric Oxygen Therapy (HBOT) is a powerful wound healing technology that utilizes specialized chambers to deliver 100% oxygen at pressures exceeding normal atmospheric pressure. This elevated oxygen concentration significantly increases the amount of oxygen dissolved in the blood plasma, promoting a cascade of healing effects within the body. HBOT supercharges tissue oxygen levels, enhancing fibroblast proliferation (cells that produce collagen), collagen synthesis (essential for wound closure), angiogenesis (new blood vessel formation), and antimicrobial activity (fighting infection). This makes HBOT particularly valuable for chronic wounds that struggle to heal with conventional methods. Modern HBOT chambers, like those from Perry Baromedical, offer a range of configurations from monoplace (single-patient) units to larger multiplace systems accommodating multiple patients simultaneously, even allowing medical staff to enter and exit during treatment.
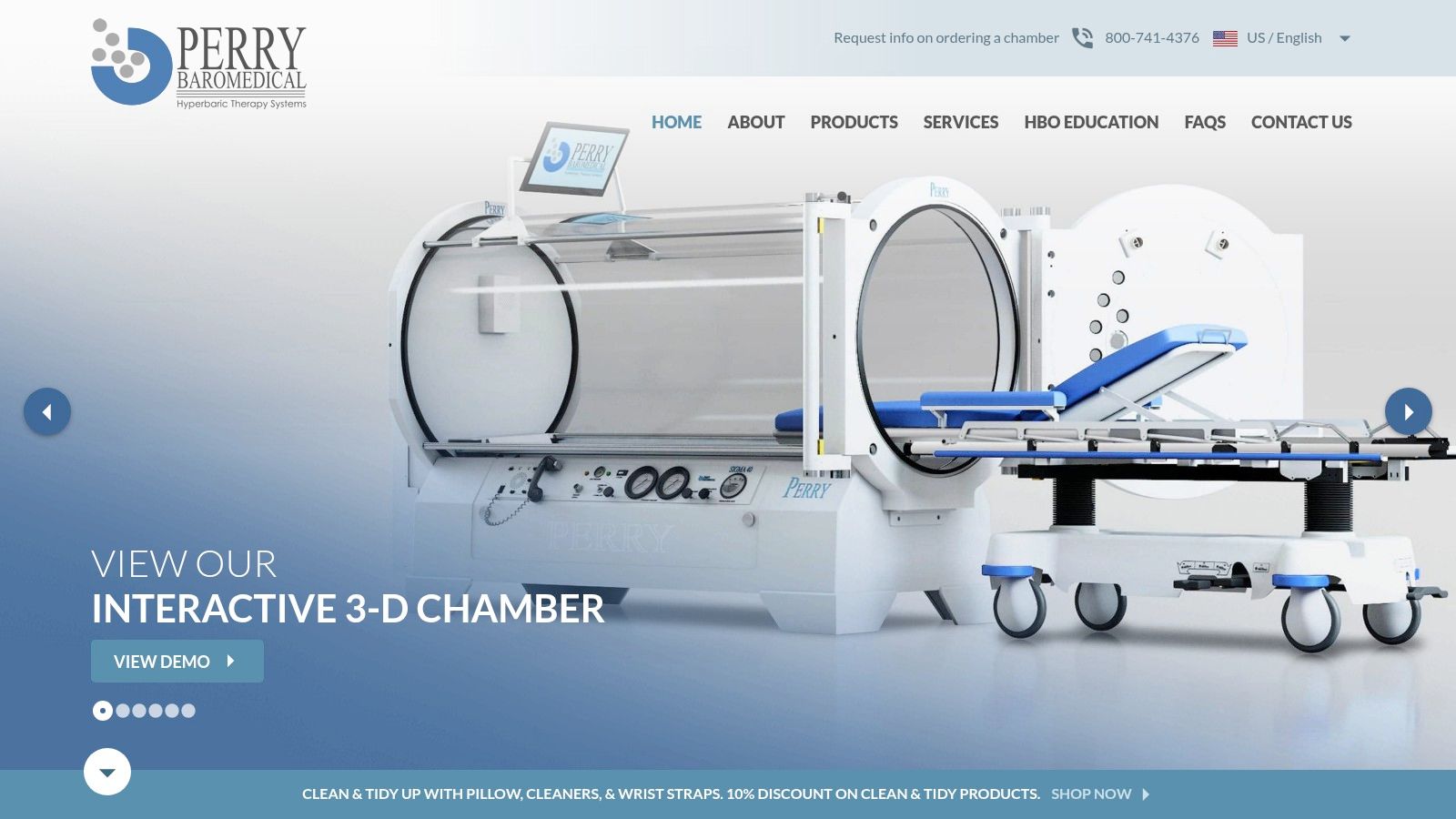
HBOT chambers play a vital role in advanced wound healing technology by addressing challenging wound types often resistant to other therapies. They are frequently employed for diabetic foot ulcers, radiation-induced tissue damage, compromised skin grafts and flaps, and certain ischemic wounds where blood supply is restricted. The intense oxygenation delivered by HBOT provides a powerful anti-inflammatory and antimicrobial effect, often salvaging compromised tissue that might otherwise require amputation. This technology offers a compelling alternative for patients facing severe wound complications, ultimately improving their quality of life and reducing long-term healthcare costs.
Features of HBOT chambers:
- Precisely Controlled Environment: Chambers maintain pressures typically between 2.0 and 2.5 atmospheres absolute (ATA), crucial for therapeutic effectiveness.
- Safety Systems: Integrated safety features include emergency decompression protocols to manage unforeseen events.
- Patient Monitoring: Vital signs are closely monitored throughout the treatment to ensure patient safety and well-being.
- Patient Comfort: Many chambers include entertainment systems such as TVs and music players to improve patient comfort during lengthy sessions.
- Advanced Climate Control: Air filtration and climate control systems maintain optimal temperature and air quality inside the chamber.
Pros of HBOT:
- Highly effective for specific wound types, especially diabetic wounds, radiation damage, and ischemic wounds.
- Demonstrates significant anti-inflammatory and antimicrobial properties.
- Can prevent amputations by promoting tissue salvage.
- Well-established reimbursement pathways exist for approved indications.
Cons of HBOT:
- High Initial Investment: HBOT chambers require a significant financial commitment, with costs ranging from $150,000 to over $1,000,000 depending on the size and features of the system.
- Time-Intensive Treatment: Treatment protocols are time-consuming, typically involving 90-120 minute sessions repeated 20-40 times.
- Risk of Barotrauma: Potential side effects include barotrauma affecting the ears, sinuses, or lungs, though these are generally mild and manageable.
- Limited Accessibility: The specialized facility requirements and high cost can limit access to HBOT for some patients.
Implementation and Setup:
Implementing HBOT requires dedicated space, specialized personnel (trained technicians and physicians), and ongoing maintenance. Facilities considering HBOT should thoroughly assess their patient population, local market demand, and financial resources. Consultation with HBOT experts and manufacturers, like Perry Baromedical (https://www.perrybaromedical.com/), is crucial during the planning and implementation stages.
HBOT earns its place on this list of wound healing technologies because of its proven efficacy in treating complex wounds, its potential to prevent limb loss, and its significant impact on patient outcomes. While the cost and time commitment can be substantial, the benefits often outweigh the challenges, especially for patients with chronic, non-healing wounds. HBOT offers a real chance for healing and improved quality of life for those who have exhausted other treatment options.
7. Ultrasound Wound Therapy Systems
Ultrasound wound therapy represents a significant advancement in wound healing technology. This innovative approach utilizes acoustic energy to stimulate tissue repair and accelerate the healing process. Low-frequency ultrasound devices, such as MIST Therapy and SonicOne, generate sound waves that produce microstreaming and cavitation effects within the wound tissues. This mechanical energy plays a crucial role in disrupting biofilms, stimulating cellular activity, increasing vascular permeability, and enhancing the delivery of growth factors essential for wound healing. These systems are particularly effective for debridement and promoting healing in chronic wounds that have stalled. For patients struggling with non-healing wounds, ultrasound therapy offers a non-invasive and often less painful alternative to traditional debridement methods.
Ultrasound wound therapy systems offer a range of features designed to optimize treatment for various wound types. Adjustable frequency and intensity settings allow clinicians to tailor the therapy to the specific needs of each patient. Both contact and non-contact delivery options are available, with some systems operating through a saline mist, further minimizing discomfort. Disposable applicator tips ensure hygienic practices and prevent cross-contamination. Importantly, these systems often come with pre-programmed treatment protocols optimized for specific wound etiologies, helping to standardize care and improve outcomes. The compact and portable design of many ultrasound wound therapy devices makes them suitable for use in various settings, from clinics and hospitals to long-term care facilities and even patients' homes, increasing access to this advanced wound healing technology.
One of the key advantages of ultrasound wound therapy is its effectiveness in debridement with minimal pain, especially compared to mechanical debridement methods, which can be quite uncomfortable. This makes it a valuable option for fragile tissues that cannot tolerate more aggressive forms of debridement. Moreover, the ability of ultrasound to disrupt bacterial biofilms, a major contributing factor to chronic wound development, significantly enhances healing potential. It can also be combined with topical antimicrobials or growth factors for enhanced delivery directly to the wound bed. This synergistic approach can optimize healing outcomes, especially in complex or challenging wounds.
While ultrasound wound therapy offers numerous benefits, it's essential to be aware of the associated costs and potential limitations. The per-treatment cost can range from $100 to $200 per session, making it a relatively expensive option. Multiple treatments over extended periods are typically required to achieve maximum benefit, adding to the overall cost of care. The effectiveness of the therapy can also vary depending on the operator's technique and experience. Furthermore, ultrasound wound therapy is contraindicated for use over electronic implants, malignancies, or areas of active bleeding. Patients and healthcare providers should carefully consider these factors when evaluating treatment options.
For more information on DermaPACE System, a specific ultrasound wound therapy device, please visit https://sanuwave.com/dermapace/. This resource provides detailed information about this particular wound healing technology and its application in various clinical settings.
8. Smart Wound Monitoring Systems
Smart wound monitoring systems represent a significant advancement in wound healing technology. These systems leverage sensor technology, advanced imaging techniques, and data analytics to provide real-time, objective assessments of wound healing progress – all without the need for disruptive dressing removal. This non-invasive approach offers numerous benefits for patients and healthcare providers alike, making it a valuable tool in modern wound care. By capturing detailed information about the wound, these systems empower clinicians to make evidence-based treatment decisions, facilitating timely interventions and personalized care plans.
Platforms like WoundVision and eKare inSight exemplify the capabilities of smart wound monitoring. They utilize multispectral imaging, thermal mapping, and sophisticated AI algorithms to track key wound characteristics such as dimensions (area, volume, and depth using 3D imaging), tissue composition (differentiating between granulation, slough, and necrotic tissue through classification algorithms), and the presence of infection markers. This data is then analyzed to provide insights into the healing trajectory, enabling proactive intervention for potential complications. Integration with electronic health records allows for seamless longitudinal tracking, while secure cloud-based storage facilitates remote monitoring and telemedicine consultations, especially beneficial for patients in rural areas or those managing their wounds at home. Machine learning algorithms further enhance the system by predicting healing outcomes and recommending personalized interventions.
For patients, especially those with chronic wounds or limited mobility, smart wound monitoring offers reduced discomfort from frequent dressing changes and the convenience of remote monitoring. For primary care providers, long-term care facilities, and wound care specialists, these systems provide objective data for accurate assessment, reducing subjectivity and enabling earlier detection of wound deterioration that might not be visible to the naked eye. This early detection is crucial for preventing complications and improving patient outcomes. Comprehensive documentation generated by these systems also simplifies reporting for insurance and regulatory compliance, a key benefit for Medicare and insurance beneficiaries. Learn more about Smart Wound Monitoring Systems
While the benefits are substantial, it's important to consider the potential drawbacks. The initial investment cost for imaging hardware and software licenses can be significant. Furthermore, proper training is essential for accurate image capture and system operation. Validation across all wound types and skin tones is an ongoing process, and some systems may have limitations in this regard. Finally, as with any cloud-based data storage, patient privacy is a critical consideration.
Despite these challenges, the potential of smart wound monitoring systems to revolutionize wound care is undeniable. By providing real-time, objective data, these systems empower clinicians to make informed decisions, personalize treatment plans, and ultimately improve the lives of patients living with acute or chronic wounds. You can explore more about eKare inSight's platform at https://ekare.ai/. While specific pricing information isn't readily available, contacting the company directly is recommended for detailed quotes based on individual needs and facility size. Technical requirements will also vary depending on the chosen system and its features, but generally include a compatible computer, internet access, and potentially specific camera hardware.
Wound Healing Tech: 8-Device Comparison
| Service / Product | Core Features & Therapies | User Experience & Quality ★ | Value & Pricing 💰 | Target Audience 👥 | Unique Selling Points ✨ |
|---|---|---|---|---|---|
| 🏆 Rapid Wound Care | Personalized home visits; advanced debridement; NPWT | ★★★★★ Rapid response ≤24h | 💰 Insurance-supported | Elderly, chronic & acute wounds | ✨ At-home & LTC care; Medicare Part B |
| Negative Pressure Wound Therapy | Vacuum-assisted healing; specialized foam/gauze dressings | ★★★★ Effective edema & bacteria control | 💰 $100-200/day | Chronic, post-surgical wounds | ✨ Portable units; digital monitoring |
| Advanced Wound Dressings (Growth Factors) | Bioactive proteins; controlled release; antimicrobial | ★★★★ Targets molecular healing | 💰 ~$1,200/tube | Diabetic foot ulcers, stalled wounds | ✨ Stimulates cell proliferation |
| Bioengineered Skin Substitutes | Living cells; structural matrix; multi-layered | ★★★★ Immediate large wound coverage | 💰 $1,500-$3,000 per application | Complex, large wounds | ✨ Tissue regeneration; reduced infection |
| Electrical Stimulation Devices | Adjustable currents; non-invasive electrodes | ★★★ Variable evidence; easy to combine | 💰 Variable; inconsistent coverage | Chronic stalled wounds, adjunct | ✨ Antimicrobial effect; portable design |
| Hyperbaric Oxygen Therapy Chambers | High-pressure oxygen; monitored environment | ★★★★ Effective for ischemic wounds | 💰 $150k-$1M infrastructure | Diabetic, radiation wounds | ✨ Powerful angiogenesis; anti-inflammatory |
| Ultrasound Wound Therapy Systems | Acoustic energy; microstreaming; debridement | ★★★★ Gentle, effective debridement | 💰 $100-$200/session | Stalled, chronic wounds | ✨ Biofilm disruption; portable |
| Smart Wound Monitoring Systems | 3D imaging; AI analytics; cloud storage | ★★★★ Remote monitoring; precise data | 💰 High initial hardware/software | Providers, remote patients | ✨ AI prediction; EHR integration |
The Future of Wound Care is Here
From rapid wound care to smart monitoring systems, the advancements in wound healing technology discussed in this article offer a glimpse into a future where wound care is more effective, less painful, and more personalized than ever before. We've explored key innovations like negative pressure wound therapy (NPWT), advanced dressings with growth factors, bioengineered skin substitutes, electrical stimulation, hyperbaric oxygen therapy, ultrasound therapy, and smart wound monitoring. These tools provide healthcare practitioners with a wider array of options to address various wound types and severities, ultimately leading to improved patient outcomes.
Choosing the right wound healing technology depends on several factors, including the type of wound, the patient's overall health, and the resources available. For instance, while NPWT might be ideal for deep or complex wounds, advanced dressings could be more suitable for superficial injuries. Similarly, smart monitoring systems can provide valuable data for chronic wounds, enabling proactive adjustments to treatment plans. For those looking to speed up their recovery, there are several scientifically-backed methods to how to accelerate wound healing from PEPTYS. When implementing these technologies, factors like proper training, patient education, and ongoing monitoring are crucial for maximizing effectiveness and minimizing complications.
The future of wound care is not just about technological advancements; it's about empowering individuals and healthcare professionals with the tools and knowledge to achieve optimal healing. With continued research and development in wound healing technology, we can anticipate even more innovative solutions that will transform the lives of those affected by acute and chronic wounds. For a streamlined and efficient approach to wound care management, explore the benefits of Rapid Wound Care, a cutting-edge platform designed to integrate and optimize various wound healing technologies. Learn more about how Rapid Wound Care can revolutionize your wound care practice.

