The Evolution of Wound Assessment Charts in Modern Care
Wound assessment charts have become essential tools in modern wound care. They've evolved from simple documentation methods into dynamic resources that guide clinical decisions and improve patient outcomes. In the past, wound documentation was often inconsistent and subjective, making it difficult to track healing progress and communicate effectively between healthcare providers.
This lack of standardization made it hard to identify best practices and measure treatment effectiveness. Structured wound assessment charts address these challenges by providing a consistent framework for evaluating and documenting wound characteristics.
This standardized documentation has significantly improved communication and collaboration among healthcare professionals. A clear, comprehensive wound assessment chart ensures that nurses, physicians, and wound care specialists all have the same understanding of a patient's wound status.
This shared understanding leads to more informed treatment decisions and ensures continuity of care. This is especially important in settings like Rapid Wound Care, where coordinated efforts between primary care providers and specialists are crucial for effective at-home wound management.
Historically, the creation of standardized wound assessment tools has been vital for successful wound management. A key advancement was the introduction of the TIME framework in 2002. TIME stands for Tissue, Infection/Inflammation, Moisture, and Edge. It offers a structured approach to assessing and managing chronic wounds.
By focusing on these key components, clinicians can systematically evaluate and address obstacles to wound healing. For example, a wound that isn't healing despite optimal patient care might indicate the need for advanced therapies. The TIME framework's emphasis on regular assessment and intervention ensures that care is tailored to each patient's specific needs, promoting optimal healing. Learn more here.
Why Standardized Wound Assessment Matters
Standardized wound assessment charts enable clinicians to spot subtle changes in wound condition that might otherwise be missed. This early detection is crucial for preventing complications and ensuring prompt intervention. These charts act as a roadmap for healing, providing a clear picture of the wound's progress and guiding necessary treatment adjustments.
These charts also contribute to better patient outcomes by ensuring consistent, evidence-based care. With a standardized approach, clinicians can more accurately track the healing trajectory and make informed decisions about the most appropriate interventions. This results in faster healing, fewer complications, and higher patient satisfaction. Wound assessment charts aren't just documentation tools; they're instruments of change, transforming how we approach wound care and improving patients' lives.
Key Components That Make Wound Assessment Charts Work
Effective wound assessment charts are more than just a record of a wound's size. They capture vital information that guides clinical decisions and promotes efficient healing. These charts offer a structured way to evaluate various wound aspects, ensuring no crucial detail is missed. This thorough documentation is the foundation of effective wound management.
Essential Elements of a Wound Assessment Chart
A well-designed wound assessment chart includes several key elements. Accurate wound measurement is essential, requiring precise documentation of length, width, and depth. This allows clinicians to track size changes over time and monitor the healing process. Characterizing the wound bed tissue is also crucial. Noting the presence of necrotic tissue, slough, granulation tissue, and epithelialization helps determine the healing stage and guides appropriate treatment.
Periwound skin assessment is another key element. Checking the skin around the wound for signs of maceration, erythema, or induration can identify potential complications and inform dressing choices. Assessing the wound exudate is also important. Documenting the type, amount, color, and odor of exudate offers valuable insights into the wound's condition and the possibility of infection.
Finally, recording pain levels is vital for patient comfort and overall well-being. Using a standardized pain scale helps track pain management effectiveness and allows for adjustments to treatment as needed. Together, these elements create a comprehensive understanding of the wound's status, leading to better clinical decisions.
To understand these elements in more detail, refer to the table below:
Core Elements of Wound Assessment Charts
A comprehensive breakdown of the essential components that should be included in any wound assessment chart, with explanations of their clinical significance.
| Assessment Component | Description | Clinical Significance | Documentation Tips |
|---|---|---|---|
| Wound Measurement | Length, width, and depth of the wound | Tracks changes in wound size and monitors healing progress | Use a ruler or measuring tape for accuracy. Document in centimeters (cm). |
| Wound Bed Tissue | Characteristics of the tissue within the wound (e.g., necrotic, slough, granulation, epithelialization) | Determines the stage of healing and guides interventions | Describe the color, texture, and percentage of each tissue type present. |
| Periwound Skin | Condition of the skin surrounding the wound | Identifies potential complications like maceration, erythema, or induration | Note any changes in color, temperature, or texture. |
| Wound Exudate | Type, amount, color, and odor of wound drainage | Provides insights into the wound's condition and potential infection | Describe the characteristics of the exudate and measure the amount. |
| Pain Level | Patient's reported pain level | Essential for patient comfort and guides pain management strategies | Use a standardized pain scale (e.g., numerical rating scale) to assess and document pain. |
This table summarizes the key components of a wound assessment chart, providing a practical guide for documentation. Using these elements ensures consistent and comprehensive wound assessments.
Why Overlooked Elements Matter
Often overlooked elements can significantly impact wound healing. Nutritional status, for example, is essential for tissue repair. A patient's nutritional intake should be documented, and any deficiencies addressed. Similarly, documenting patient mobility helps determine pressure relief needs and prevents further problems. Assessing bioburden or infection is also critical. Signs of infection, such as increased exudate, foul odor, or surrounding inflammation, should be carefully documented and treated promptly. The development of wound assessment charts reflects the wider adoption of digital solutions, such as workflow automation in healthcare. This move toward digital documentation further improves the accuracy and efficiency of wound assessments.
Comprehensive Documentation: The Key to Exceptional Wound Management
Including photography in wound assessment charts provides valuable visual records of the wound's progress, enabling more accurate tracking of changes and improving communication between healthcare providers. Documenting any underlying medical conditions, such as diabetes or vascular disease, is also crucial, as these can greatly influence healing. These additional components, along with the core elements, create a comprehensive assessment that guides effective treatment and promotes optimal patient outcomes.
The TIME Framework: Transforming Wound Assessment Practices
The TIME framework has become essential for wound assessment charting. It provides a structured way to evaluate and manage wounds. This framework—Tissue, Inflammation/Infection, Moisture, and Edge—guides clinicians through a systematic assessment. This transforms subjective observations into actionable treatment plans. Clinicians using TIME-based charts identify healing barriers 68% faster and make better treatment choices.
Tissue: The Foundation of Healing
The first element, Tissue, focuses on evaluating the wound bed. This involves identifying the type of tissue present (necrotic, slough, granulation, epithelial) and its condition. Accurate tissue assessment guides decisions about debridement, the removal of non-viable tissue. For example, necrotic tissue often needs sharp debridement. Slough might require enzymatic debridement.
Inflammation/Infection: Detecting Early Warning Signs
Inflammation, the second component, emphasizes detecting infection. Clinicians look for signs of erythema, edema, warmth, and increased exudate. Managing inflammation is crucial for preventing infection, a major barrier to healing. Even small inflammation changes can indicate a developing problem. This highlights the importance of thorough wound assessment chart documentation.
Moisture: Balancing the Healing Equation
Proper Moisture balance is critical. Too much moisture can cause maceration. Too little moisture can hinder cell migration and tissue regeneration. The wound assessment chart helps clinicians evaluate moisture levels and select appropriate dressings. A highly exudative wound needs an absorbent dressing. A dry wound benefits from a hydrating dressing. This personalized approach optimizes healing.
Edge: Uncovering Barriers to Closure
The final element, Edge, involves assessing the wound margins. Clinicians examine the edges for undermining, rolling, or epibole. These can hinder epithelialization, the process of new skin growth. Understanding the wound edge helps determine interventions to promote closure. This might involve specialized dressings or other treatments to stimulate cell growth.
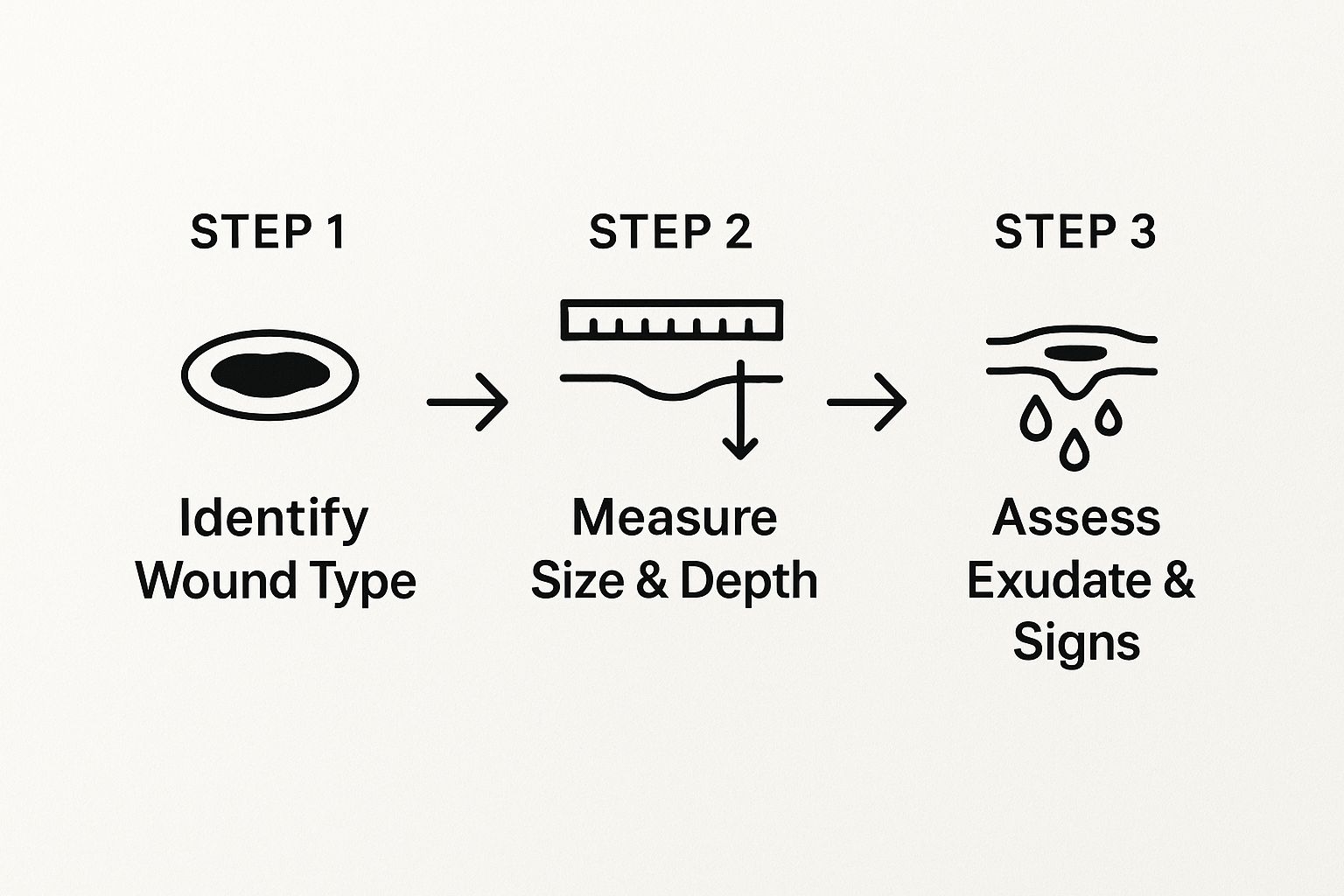
This infographic shows the steps involved in a thorough wound assessment. It starts with identifying the wound type. Then, it shows precisely measuring its dimensions. Finally, it illustrates assessing the exudate and other clinical signs. This process ensures a systematic approach, leading to better diagnosis and treatment planning.
The TIME framework and wound assessment charts have changed how we approach wound healing. They provide a consistent, evidence-based approach. This methodology continually adapts to new wound care technologies while maintaining its core principles. This allows clinicians to give the most effective, personalized care, leading to improved patient outcomes.
Turning Documentation Into Better Patient Outcomes
Wound assessment charts are essential for positive patient outcomes. They are more than just a regulatory requirement; they are a cornerstone of effective wound care. Proper documentation directly correlates with faster healing, fewer complications, and increased patient satisfaction. This means using a wound assessment chart correctly can significantly improve a patient's healing experience.
Early Detection and Timely Intervention
Using wound assessment charts consistently allows clinicians to detect subtle changes in a wound's condition, often days earlier than they would without them. For example, a small increase in exudate or a change in wound bed color, documented consistently, can alert a clinician to a developing infection before it becomes serious. This early identification allows for quick intervention, preventing major complications down the line.
Thorough documentation also helps avoid unnecessary hospitalizations. By closely monitoring wound progress, clinicians can adjust treatment plans as needed, often preventing the need for more intensive care. This leads to better outcomes for patients and substantial cost savings for healthcare systems.
Standardized Care and Reduced Variability
Facilities using comprehensive wound assessment protocols see noticeable improvements in the quality of care. Some organizations report a 43% reduction in treatment variability after implementing standardized wound assessment charts. This consistency is vital because it ensures that all patients receive evidence-based care, no matter which clinician is providing the treatment. This means patients experience more predictable and dependable healing.
Furthermore, wound assessment is crucial in identifying factors that hinder healing. A significant number of wounds, impacting up to 30% of patients with chronic wounds, are complicated by underlying conditions like diabetes and vascular diseases, significantly affecting healing rates. In the United States alone, over 6.5 million people suffer from chronic wounds, costing more than $25 billion annually. Effective wound assessment tools, like the Bates-Jensen Wound Assessment Tool (BWAT), help clinicians systematically document and monitor these factors. Learn more about comprehensive wound assessment here.

Bridging Communication Gaps
Wound assessment charts also act as a vital communication tool between different care settings. When a patient moves from the hospital to a rehabilitation facility or home healthcare, the wound assessment chart provides a complete record of the wound's history and current status. This ensures continuity of care and prevents the loss of important information during transitions. Services like Rapid Wound Care benefit from this continuity, as it facilitates effective at-home wound management through clear communication between primary care providers, specialists, and patients.
Consistent documentation, using wound assessment charts, truly changes wound care for the better. It results in earlier interventions, reduces complications, and improves overall patient well-being. By using these valuable tools, we can improve the standard of wound care and make a real difference in the lives of patients. This proactive approach to wound management is essential for optimizing healing and improving patient outcomes.
Digital vs. Paper: Choosing Your Wound Assessment Solution

Documenting wounds has entered a new era. While paper charts have long served as the standard, digital wound assessment platforms are gaining traction. Both methods offer distinct advantages and disadvantages. Making an informed choice depends on understanding these key differences and selecting the solution that best suits your specific needs.
The Benefits of Digital Wound Assessment Charts
Digital wound assessment charts bring a host of benefits to modern wound care. A primary advantage is automated measurement. Digital platforms calculate wound area and volume directly from photographs. This eliminates manual errors and saves significant time, ultimately increasing the accuracy of assessments. Integrated photography is another valuable feature, allowing easy storage, retrieval, and comparison of images, documenting the healing journey visually.
Digital systems also excel at trend analysis visualization. Clear charts and graphs illustrate healing progress, allowing for early identification of potential issues. When exploring digital options, consider the value of a comprehensive dashboard, like a Product Performance Dashboard, to enhance data analysis and reporting capabilities. These features make digital charts a powerful asset in improving wound care.
The Advantages of Paper-Based Approaches
Despite the advancements of digital solutions, paper-based wound assessment charts remain relevant. They offer crucial accessibility in settings with limited technology or unreliable internet access. This makes them practical for smaller clinics or home healthcare environments. Some clinicians also prefer the tactile nature of paper charts, finding them simpler for detailed observations or quick notes during patient visits.
However, paper charts present storage challenges. They are bulky and susceptible to damage or loss. This is a critical factor when choosing the best method for your practice.
To help visualize the key differences, let's take a look at the following comparison:
Digital vs. Paper Wound Assessment Charts
A detailed comparison of digital and paper-based wound assessment systems, highlighting the strengths and limitations of each approach.
| Feature | Digital Charts | Paper Charts | Clinical Considerations |
|---|---|---|---|
| Accessibility | Requires devices and internet access | Readily available | Consider technology infrastructure and resources |
| Data Management | Automated measurements, integrated photography, trend analysis | Manual measurements, separate photo storage, manual trend analysis | Evaluate the need for accurate measurements and efficient data analysis |
| Storage & Security | Electronic storage, data backups, access controls | Physical storage, susceptible to damage and loss | Assess data security and storage capacity needs |
| Workflow Integration | Can integrate with EHR systems | Requires manual data entry into EHR | Determine the importance of streamlined documentation and interoperability |
| Cost | Software subscriptions, hardware costs | Chart printing costs, physical storage space | Analyze long-term cost-effectiveness and return on investment |
This table highlights the core differences between digital and paper charting, emphasizing the importance of considering clinical needs and available resources. Digital charts offer advanced features for data management and integration, while paper charts provide immediate accessibility.
Integrating Digital Charts with EHR Systems
Leading healthcare facilities are integrating digital wound assessment charts with their Electronic Health Record (EHR) systems. This integration streamlines documentation workflows. Assessment data automatically flows into the patient's EHR, reducing transcription errors and saving administrative time. This connectivity ensures all care team members access the most current wound information.
A crucial advantage of EHR integration is the improvement in assessment quality. Digital platforms prompt clinicians to complete all required fields, ensuring thorough documentation and minimizing missed information. This systematic approach enhances the overall standard of care.
Addressing Implementation Challenges
Implementing digital wound assessment charts can present obstacles. Staff resistance to new technology is a common hurdle. Effective training and ongoing support facilitate clinician adaptation. Adequate training is essential for clinicians to comfortably use the digital platform and input data accurately.
Addressing connectivity issues is also vital. Reliable internet access is paramount for digital wound assessment. Facilities may need infrastructure upgrades to ensure smooth operation. These strategies can mitigate potential issues and support a seamless transition.
Emerging Technologies: 3D Wound Imaging and AI
The future of wound assessment holds exciting advancements. 3D wound imaging is transforming wound visualization and measurement, offering highly precise data that tracks minute changes in wound volume and surface area. AI-assisted assessment is another innovative area. AI algorithms analyze wound images, identifying tissue types, detecting infection signs, and even predicting healing trajectories.
These technologies are continuously developing, but their potential to enhance the accuracy and efficiency of wound documentation is undeniable, ultimately leading to improved patient outcomes.
Implementing Wound Assessment Charts That Actually Work
Choosing the right wound assessment chart is just the first step. Successfully integrating it into practice requires careful planning and staff buy-in. We'll explore how wound care leaders have successfully transformed their documentation practices, overcoming common obstacles like documentation fatigue and inconsistent use.
Conducting Effective Needs Assessments
Begin by assessing your organization's specific needs. What are your current documentation practices? What challenges are you facing? What are your goals for implementing wound assessment charts?
For example, are you aiming to improve healing rates, reduce complications, or streamline documentation? Understanding your starting point and desired outcomes is crucial for successful implementation. This assessment lays the groundwork for selecting the right tools and strategies.
Selecting Champions and Building Support
Identify key individuals within your organization who will champion the adoption of wound assessment charts. These champions should be respected by their peers and passionate about improving wound care. They will be instrumental in promoting the benefits of the new charts and encouraging their colleagues to embrace the change.
Building a strong support network is essential for overcoming resistance to new processes. This support creates a positive environment for implementation.
Developing Targeted Training Programs
Training programs should be tailored to the specific needs of your staff. Consider different learning styles and offer a variety of training formats. Some examples include online modules, hands-on workshops, and one-on-one coaching.
For instance, nurses comfortable with digital tools may only need a brief overview of the new software. Those less tech-savvy may benefit from more in-depth training. Effective training ensures everyone feels confident using the new wound assessment charts.
Creating Practical Documentation Policies
Develop clear, concise policies that outline how wound assessment charts should be used. These policies should balance the need for comprehensive documentation with the realities of clinical workflow.
For example, consider using a simplified charting system for routine wound assessments. Reserve more detailed charts for complex wounds. Practical policies encourage consistent use and prevent documentation fatigue. This balance optimizes documentation practices.
Measuring Compliance and Refining Your Approach
Regularly monitor compliance with documentation policies and gather feedback from staff. Are the charts being used consistently? Are they capturing the necessary information? Are there any areas where the process can be improved?
For example, if staff find the charts too time-consuming, explore ways to simplify them without sacrificing essential data. Continuous refinement based on real-world feedback is essential for maximizing the effectiveness of wound assessment charts.
Actionable Timelines and Metrics for Success
Creating an implementation timeline with specific milestones and measurable goals will help track progress and ensure accountability. For example, you might set a goal of achieving 90% compliance with documentation policies within three months of implementation.
Track key metrics, such as healing rates, complication rates, and patient satisfaction. These metrics demonstrate the impact of the new wound assessment charts and provide a tangible measure of success.
For patients seeking effective and personalized wound care solutions, consider Rapid Wound Care. We offer comprehensive at-home wound care services, providing advanced therapies and a patient-centered approach to healing.

