Unlocking the Secrets to Faster Skin Healing
Dealing with a wound can be frustrating. This listicle reveals seven evidence-based strategies to help skin heal quickly and minimize scarring. Whether you're a patient, caregiver, or healthcare professional, understanding these methods can significantly improve healing outcomes. Learn how proper wound cleaning, aloe vera, medical-grade honey, zinc, growth factor therapies, hyperbaric oxygen therapy (HBOT), and low-level laser therapy (LLLT) can help answer what helps skin heal quickly and promote effective recovery.
1. Proper Wound Cleaning and Dressing
When it comes to figuring out what helps skin heal quickly, proper wound cleaning and dressing is paramount. It's the foundation upon which all other healing processes build. This involves gently cleaning the affected area to remove debris and bacteria that can hinder healing. This cleaning should be done with mild soap and water, or a saline solution, followed by the application of an appropriate dressing. Maintaining a moist wound environment is key, as research shows that moist wound healing accelerates epithelialization (skin cell regrowth) by up to 50% compared to dry healing.
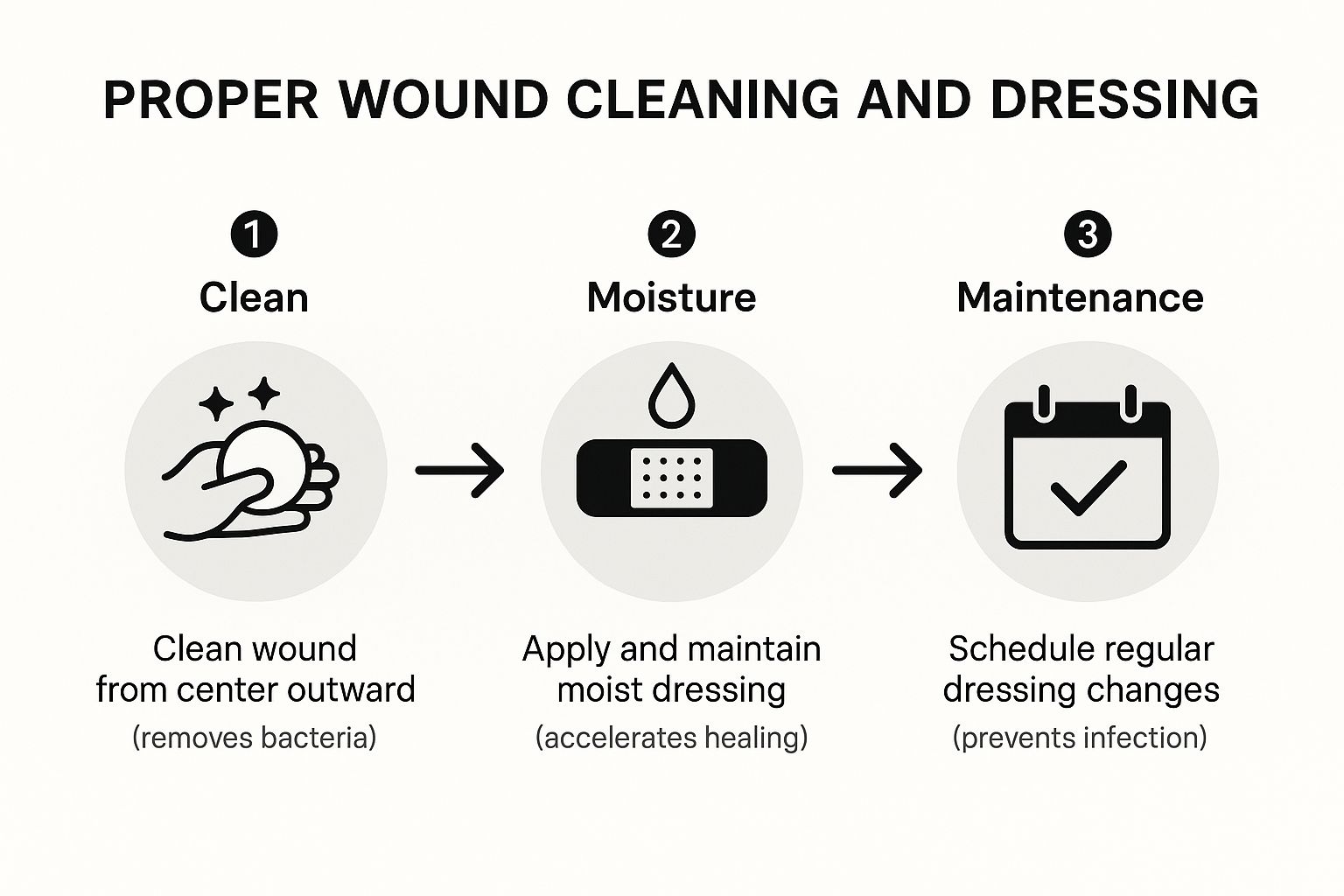
The infographic above illustrates the crucial steps involved in proper wound care. It begins with stopping the bleed, followed by cleaning the wound with mild soap and water or saline solution. Next, a topical antibiotic ointment can be applied (if recommended by a healthcare professional), followed by covering the wound with a sterile dressing. Finally, the infographic emphasizes the importance of changing the dressing regularly. The sequence highlighted in this infographic ensures the wound is protected from further contamination and promotes optimal healing. Understanding the stages of wound healing can help you take better care of your skin and support its natural healing process as explained by PEPTYS in their guide "Ako urýchliť hojenie rany: Overený sprievodca pre rýchlejšiu regeneráciu tkanív".
This simple yet effective approach offers numerous benefits: it removes bacteria and contaminants, creates an optimal moisture balance for cell migration, provides physical protection from external irritants, and significantly reduces the risk of infection and scarring. Studies at Stanford University, for example, have shown that moist wound environments can increase healing rates by 30-50%, echoing the importance of this method. Hospital protocols universally emphasize proper wound cleaning and dressing as the foundation of wound care.
Pros:
- Accelerates healing time significantly
- Reduces pain during the healing process
- Minimizes scarring potential
- Relatively inexpensive and accessible
Cons:
- Requires regular dressing changes
- Can be technique-sensitive; incorrect cleaning can damage new tissue
- Can be time-consuming as part of a daily care routine
Tips for Effective Wound Cleaning and Dressing:
- Clean wounds with gentle motions from the center outward.
- Use lukewarm water rather than hot water.
- Change dressings according to manufacturer recommendations.
- Consider semi-occlusive dressings like hydrocolloids for optimal moisture balance.
This approach deserves its place on this list because it's the first and most crucial step in facilitating rapid skin healing. Pioneering research by Dr. George Winter on moist wound healing, along with widely recognized products like Band-Aid (Johnson & Johnson) and Tegaderm (3M), further solidify its importance. Whether dealing with a chronic wound or an acute injury, proper wound cleaning and dressing sets the stage for efficient and effective recovery.
This video provides a visual demonstration of proper wound cleaning and dressing techniques. It's a valuable resource for patients, caregivers, and healthcare professionals alike.
2. Aloe Vera Gel
When considering what helps skin heal quickly, aloe vera gel quickly rises to the top of the list. This clear gel, derived from the succulent aloe vera plant, has been a staple in wound care for millennia. Its remarkable healing properties stem from a rich composition of over 75 active compounds, including vitamins, enzymes, minerals, sugars, lignin, saponins, and amino acids. These components work synergistically to address various aspects of skin healing, making it a versatile and effective natural remedy.

Aloe vera's healing power lies in its ability to reduce inflammation, stimulate collagen production, and enhance the cross-linking of collagen fibers. This multifaceted approach accelerates wound contraction, strengthens the newly formed scar tissue, and minimizes the risk of complications. Two key compounds, glucomannan and gibberellin, interact with growth factor receptors in the skin, further boosting the healing process. The gel's anti-inflammatory properties, provided by compounds like bradykininase, help reduce redness, swelling, and pain. Furthermore, aloe vera possesses antimicrobial properties, helping to prevent infection in minor wounds. Finally, the gel's high water content (99%) provides essential hydration to the wound site, creating an optimal environment for tissue regeneration.
The effectiveness of aloe vera in promoting skin healing is well-documented. A NASA study demonstrated that aloe vera improved the healing of radiation burns by an impressive 36%. Furthermore, a 2018 clinical trial showed a 50% faster healing time for first-degree burns treated with aloe vera compared to standard care. These findings highlight the potential of aloe vera as a valuable tool in various wound care settings, from treating minor burns and scrapes to supporting the healing of more complex skin injuries.
Pros:
- Widely accessible and affordable: Aloe vera gel is readily available in most pharmacies and health stores, making it an economical option for wound care.
- Natural and safe: As a natural remedy, aloe vera has minimal side effects, making it suitable for a wide range of individuals.
- Easy home cultivation: You can easily grow your own aloe vera plants at home for a readily available source of fresh gel.
- Pain relief and healing: Aloe vera offers dual benefits by soothing pain and simultaneously promoting faster healing.
Cons:
- Variable potency: The potency of commercially available aloe vera products can vary significantly.
- Allergic reactions: Some individuals may experience allergic reactions to aloe vera.
- Oxidation of fresh gel: Freshly extracted aloe vera gel oxidizes quickly, reducing its effectiveness if not used immediately.
- Limitations for deep wounds: While effective for minor wounds, aloe vera is not a substitute for medical treatment for deep or severe wounds.
Tips for Effective Use:
- Fresh is best: For maximum potency, extract the gel directly from fresh aloe vera leaves.
- Refrigerate for soothing effect: Store aloe vera gel in the refrigerator for an extra soothing and cooling effect upon application.
- Regular application: Apply aloe vera gel to clean wounds 2-3 times daily for optimal results.
- Choose high-quality products: Look for commercial products containing at least 95% pure aloe vera with minimal additives.
Aloe vera's historical use, combined with scientific evidence supporting its efficacy, solidifies its position as a valuable aid in skin healing. For patients with chronic or acute wound conditions, primary care providers, long-term care facilities, wound care specialists, and even elderly patients seeking natural remedies, aloe vera gel offers a safe, accessible, and effective option to promote faster healing and reduce discomfort. From its use by the Ancient Egyptians, who called it the "plant of immortality," to modern research and commercialization by companies like Forever Living Products and innovators like Dr. Bill C. Coats, aloe vera continues to be a powerful tool in promoting skin health and accelerating the healing process.
3. Medical-Grade Honey
When considering what helps skin heal quickly, medical-grade honey deserves a prominent place in the conversation. Unlike the honey you find in your pantry, medical-grade honey, often Manuka honey from New Zealand, is sterilized and prepared specifically for wound healing. This unique substance harbors a wealth of bioactive compounds, including high concentrations of methylglyoxal, which create an environment conducive to healing and hostile to bacteria. It fosters rapid skin recovery by creating an acidic, high-osmolarity environment that draws fluid away from the wound, inhibiting bacterial growth and promoting tissue regeneration. The honey forms a protective barrier, maintaining optimal wound moisture while simultaneously delivering these potent healing compounds.

Medical-grade honey’s efficacy stems from several key features. Its potent antibacterial properties combat even antibiotic-resistant strains, making it a valuable tool in the fight against increasingly resilient infections. The osmotic effect draws excess fluid from the wound, reducing swelling and promoting a cleaner healing environment. A low pH further inhibits bacterial growth, while the release of hydrogen peroxide provides continuous antimicrobial action. Furthermore, naturally occurring enzymes within the honey aid in debridement, gently removing dead tissue without harming healthy cells, thereby accelerating the healing process.
This approach offers several advantages for patients and healthcare providers alike. It effectively combats biofilms and antibiotic-resistant bacteria, a growing concern in wound care. It significantly reduces wound odor, improving patient comfort and quality of life. Minimized dressing changes mean less pain and disruption for the patient, while also reducing nursing time and overall healthcare costs. The natural debriding action contributes to a cleaner wound bed and faster healing.
While highly effective, medical-grade honey does have some drawbacks. It is typically more expensive than conventional wound treatments. Application can be messy without the use of proper dressings, and some individuals may experience a mild stinging sensation upon application. Importantly, it is contraindicated for those with bee allergies.
The effectiveness of medical-grade honey is supported by a growing body of clinical evidence. A 2020 systematic review found medical honey more effective than silver sulfadiazine, a commonly used topical antimicrobial, for burn healing. The UK National Health Service now regularly uses Manuka honey dressings for chronic wounds, and clinical studies demonstrate an impressive 85% success rate in healing chronic leg ulcers resistant to other treatments. Pioneering research by Professor Peter Molan has significantly advanced our understanding of medical honey's therapeutic potential, and leading brands like Comvita and Medihoney have made these products readily available.
For those seeking to leverage the healing power of medical-grade honey, a few practical tips can ensure optimal results. Look for a UMF (Unique Manuka Factor) rating of 10+ for wound care. Apply a thin layer directly to the wound or use honey-impregnated dressings. Cover with a secondary dressing to prevent messiness and maintain a sterile environment. For maximum benefit, leave the honey on the wound for at least 12 hours before changing the dressing.
Medical-grade honey offers a compelling solution for individuals seeking to accelerate skin healing. Its remarkable antibacterial properties, combined with its ability to promote a healthy wound environment, make it a valuable option for a wide range of wound types, particularly those that have proven resistant to other therapies. From chronic leg ulcers to burns, medical-grade honey presents a natural and effective pathway to faster, more comfortable healing.
4. Zinc Supplementation: Fueling Your Skin's Repair Mechanisms
If you're looking for what helps skin heal quickly, ensuring adequate zinc levels is crucial. Zinc, a vital micronutrient, plays a starring role in numerous cellular processes critical for skin regeneration and overall health. From immune function and protein synthesis to DNA synthesis and cell division, zinc is the engine driving efficient wound healing. Deficiencies in this essential mineral can significantly impair the body's ability to repair damaged skin, making supplementation a valuable tool in accelerating recovery. This is particularly true for individuals with suboptimal zinc levels, whether due to dietary factors, age, or underlying health conditions.
Zinc's contribution to wound healing is multifaceted. It acts as an essential cofactor for over 300 enzymes involved in the healing process, including matrix metalloproteinases. These enzymes are crucial for cell migration during the proliferative phase, essentially enabling the skin to rebuild itself. Furthermore, zinc bolsters immune function at wound sites, supporting the immune cells responsible for clearing debris and fighting infection, preventing complications that can delay healing. It also facilitates the protein synthesis necessary for generating new tissue and enhances collagen deposition and cross-linking, contributing to stronger, more resilient skin.
Examples of Zinc's Healing Power:
- Research at the University of Michigan demonstrated a remarkable 43% faster healing rate in elderly patients with pressure ulcers who received zinc supplementation.
- Studies involving post-surgical patients have also shown that zinc supplementation can lead to 25% faster incision healing.
Why Zinc Deserves its Place on the List:
Zinc supplementation offers a systemic approach to healing, benefiting all wounds simultaneously. It addresses a common nutritional deficiency that often goes unnoticed and significantly impairs healing. Moreover, zinc supplements are relatively inexpensive and easily accessible, making them a practical addition to any wound care regimen. Zinc supplementation can be combined effectively with other healing modalities for a comprehensive approach to skin repair.
Pros and Cons of Zinc Supplementation:
Pros:
- Addresses a common nutritional deficiency.
- Systemic effect benefits all wounds.
- Relatively inexpensive and accessible.
- Can be combined with other healing modalities.
Cons:
- Excessive supplementation can cause nausea and interfere with copper absorption.
- Benefits primarily seen in those with suboptimal zinc levels.
- Takes time to build effective tissue concentrations.
- Oral supplementation may be less effective for severe deficiency requiring medical supervision.
Actionable Tips for Using Zinc Supplementation:
- Standard supplementation ranges from 15-30mg daily. Always consult with your healthcare provider before starting any new supplement regimen, especially if you have pre-existing health conditions or are taking other medications.
- Zinc oxide topical preparations provide direct delivery of zinc to wound sites and can be beneficial for localized wounds.
- Boost your dietary intake of zinc-rich foods. Include oysters, beef, pumpkin seeds, and legumes in your diet to naturally increase your zinc levels.
- Take zinc supplements between meals with water for optimal absorption. Avoid taking zinc supplements with dairy or calcium-rich foods, as these can interfere with absorption.
Who Should Consider Zinc Supplementation?
Patients with chronic or acute wound conditions, those recovering from surgery, individuals with poor nutritional status, and the elderly are prime candidates for considering zinc supplementation as part of their overall wound healing strategy. Primary care providers, long-term care facilities, wound care specialists, and other healthcare practitioners should be aware of the benefits of zinc in promoting skin health and healing.
Pioneering Figures and Brands:
The importance of zinc in human health and wound healing was pioneered by Dr. Ananda Prasad. Reputable supplement brands like Life Extension and Nature's Way offer a variety of zinc supplements. Furthermore, the World Health Organization (WHO) includes zinc in its list of essential medicines, highlighting its global significance.
5. Growth Factor Therapies: Supercharging Skin Regeneration
When you're looking for what helps skin heal quickly, especially for stubborn or slow-healing wounds, growth factor therapies represent a significant advancement in wound care. These therapies harness the power of naturally occurring proteins called growth factors, which orchestrate the intricate process of tissue repair. By concentrating and applying these growth factors to the wound site, healing can be dramatically accelerated. This makes growth factor therapies a powerful tool for those dealing with chronic wounds or seeking faster recovery from acute injuries.
How They Work:
Growth factors are signaling molecules that essentially instruct cells to migrate, proliferate, and build new tissue. Think of them as the foremen on a construction site, directing the workers to repair damage. Different growth factors play specific roles: platelet-derived growth factor (PDGF) stimulates blood vessel formation, epidermal growth factor (EGF) promotes skin cell growth, and transforming growth factor beta (TGF-β) helps organize the new tissue. By artificially increasing the concentration of these growth factors at the wound site, we can effectively "fast-forward" the natural healing process.
Types of Growth Factor Therapies:
- Recombinant Human Growth Factors: These are laboratory-produced growth factors, identical to those found naturally in the body. A well-known example is becaplermin (Regranex) gel, often used for diabetic foot ulcers.
- Platelet-Rich Plasma (PRP): This therapy utilizes a concentrated sample of the patient's own blood plasma, which is rich in growth factors. It leverages the body's own healing potential and offers a personalized approach. PRP has gained popularity among professional athletes like Tiger Woods and Rafael Nadal for accelerating injury recovery.
Features and Benefits:
- Targeted Healing: Growth factors precisely target the biological pathways involved in healing, optimizing the entire repair process.
- Cellular Stimulation: They directly stimulate key cells involved in wound healing, including fibroblasts (which produce collagen), keratinocytes (skin cells), and endothelial cells (which form blood vessels).
- Versatile Delivery: Growth factors can be delivered via specialized dressings, injections, or topical gels, depending on the specific wound and chosen therapy.
- Reduced Scarring: By optimizing collagen organization, growth factor therapies can minimize scar tissue formation, resulting in a more aesthetically pleasing outcome.
Pros:
- Accelerated Healing: Growth factor therapies can significantly speed up healing, especially for chronic wounds that have been resistant to other treatments. Studies have shown an 80% success rate in chronic wounds that failed traditional therapy.
- Effective for Difficult Wounds: They are particularly effective for challenging wounds like diabetic ulcers, venous leg ulcers, and pressure sores. For example, Regranex gel demonstrated a 43% higher complete healing rate for diabetic foot ulcers.
- Personalized Treatment (PRP): PRP therapy allows for a personalized approach using the patient's own growth factors.
Cons:
- Cost: Growth factor therapies are generally more expensive than conventional wound care treatments.
- Insurance Coverage: They are often not fully covered by insurance, which can create a financial barrier for some patients.
- Special Handling: Some formulations require refrigeration and specific handling procedures.
- Theoretical Cancer Risk: While clinical evidence is largely reassuring, there is a theoretical risk that growth factors could promote cancerous growth. This concern is minimal with proper medical supervision.
Tips for Using Growth Factor Therapies:
- Medical Supervision: These therapies are best used under the guidance of a qualified healthcare professional.
- Proper Storage: Follow storage instructions carefully to maintain product stability.
- Combined Therapies: Growth factor therapies are often most effective when used in conjunction with advanced wound dressings and other appropriate treatments.
- Multiple Applications: Multiple applications are typically required to achieve optimal results.
Growth factor therapies offer a powerful and innovative approach to wound healing, particularly for those struggling with chronic or slow-healing wounds. While they represent a significant investment, their potential to accelerate healing and improve outcomes makes them a valuable option for many patients seeking what helps skin heal quickly. Consulting with a wound care specialist is essential to determine if growth factor therapy is the right choice for your individual needs.
6. Hyperbaric Oxygen Therapy (HBOT)
When exploring options for what helps skin heal quickly, Hyperbaric Oxygen Therapy (HBOT) emerges as a powerful, albeit specialized, treatment. This therapy involves breathing pure oxygen in a pressurized chamber, typically at pressures 2-3 times higher than normal atmospheric pressure. This environment supercharges the bloodstream with oxygen, leading to a cascade of healing benefits. The increased oxygen combats tissue hypoxia (low oxygen levels), a major impediment to healing, and reduces edema (swelling). Furthermore, HBOT enhances white blood cell function, crucial for fighting infection, stimulates angiogenesis (the formation of new blood vessels to nourish damaged tissue), and promotes fibroblast activity, which is essential for collagen production and tissue regeneration. In essence, HBOT creates the optimal oxygen environment for the body to rebuild and repair itself.

HBOT increases tissue oxygen levels up to 15 times normal, significantly boosting the body's natural healing mechanisms. This therapy dramatically enhances the bacterial killing capacity of neutrophils, a type of white blood cell, making it particularly effective against infections. The increased oxygen also directly promotes collagen production and deposition, the foundation for new skin growth. Additionally, HBOT reduces tissue edema through vasoconstriction, further optimizing the healing environment. Finally, studies suggest that HBOT can even stimulate stem cell mobilization from bone marrow, contributing to long-term tissue regeneration.
HBOT demonstrates remarkable efficacy in treating a range of wound types, especially those complicated by poor circulation. It's FDA-approved for several conditions, including diabetic foot ulcers, a common and serious complication of diabetes. The therapy is non-invasive and painless, making it a viable option for even the most fragile patients. Importantly, HBOT can be used synergistically with other wound care approaches, amplifying their effectiveness.
While highly effective, HBOT does have some drawbacks. It's expensive, with sessions typically costing between $250 and $450, and a full course of treatment often requires 20-40 sessions. The availability of hyperbaric chambers is limited in many regions, requiring patients to travel for treatment. Each session lasts 90-120 minutes, which can be a significant time commitment. Potential side effects, though rare, include ear and sinus barotrauma (pressure-related discomfort) and oxygen toxicity.
Examples of HBOT's success:
- Research shows an 89% reduction in major amputations for diabetic foot ulcers with HBOT.
- The Mayo Clinic reports an 80% improvement in radiation wound healing with HBOT.
- Military studies demonstrate 30% faster healing of combat wounds with HBOT integration.
Tips for HBOT treatment:
- Treatments are typically administered 5 days a week for 4-6 weeks.
- Avoid petroleum-based products before treatment due to the fire hazard associated with pure oxygen.
- Clear your ears frequently during pressure changes to prevent barotrauma.
- Continue standard wound care between HBOT treatments.
HBOT deserves its place on this list because it offers a significant advantage in accelerating healing for complex and challenging wounds. It addresses the root causes of delayed healing by increasing oxygen delivery, fighting infection, and stimulating tissue regeneration. While cost and accessibility can be barriers, the potential benefits, especially for patients with chronic or slow-healing wounds, make HBOT a valuable option to explore. For patients with conditions like diabetic foot ulcers, where amputation is a real risk, HBOT can be a limb-saving intervention. If you're struggling with a wound that isn't healing well, talk to your doctor about whether HBOT might be right for you.
7. Low-Level Laser Therapy (LLLT) for Accelerated Skin Healing
When searching for what helps skin heal quickly, Low-Level Laser Therapy (LLLT), also known as photobiomodulation, emerges as a promising and innovative treatment option. This therapy utilizes specific wavelengths of light to stimulate cellular function and dramatically accelerate the wound healing process. Unlike the high-powered lasers used in surgery, LLLT operates at a low power (1-500mW) and doesn't produce heat or damage surrounding tissue, making it a safe and effective method for a variety of wound types.
How Does LLLT Work?
LLLT works by delivering photons of light (typically in the red and near-infrared spectrum, 600-1000nm) deep into the skin. These photons are absorbed by cellular chromophores, primarily within the mitochondria, the powerhouses of our cells. This absorption triggers a cascade of beneficial biological effects, including increased ATP (energy) production, modulation of reactive oxygen species (reducing inflammation), and activation of transcription factors that promote cell growth and repair. The result? Increased cell proliferation and migration, along with enhanced synthesis of growth factors and extracellular matrix proteins, all essential components for rapid and effective wound healing.
Why LLLT Deserves Its Place on the List:
LLLT stands out among other wound healing methods due to its unique non-thermal, photochemical approach. It offers a range of benefits including:
- Depth of Penetration: The specific wavelength used determines the depth of penetration, ranging from 1-5cm. Red light (630-660nm) targets superficial tissues, while near-infrared light (810-850nm) reaches deeper structures, allowing for customized treatment based on the wound's location and severity.
- Improved Circulation: LLLT also stimulates the release of nitric oxide, a potent vasodilator, which increases blood flow to the injured area, delivering vital oxygen and nutrients needed for healing.
Proven Effectiveness:
The efficacy of LLLT has been demonstrated in numerous studies:
- Research at Harvard Medical School showed a 40% acceleration in surgical wound healing with LLLT.
- NASA studies demonstrated a remarkable 155-171% increase in cell growth rates using LED photobiomodulation.
- A 2018 meta-analysis of 22 studies confirmed significant acceleration of wound healing across diverse wound types, further solidifying its potential.
Pros and Cons:
Pros:
- Non-invasive and painless
- No known side effects when properly administered
- Can be used on infected wounds without spreading infection
- Compatible with virtually all other treatment modalities
Cons:
- Equipment can be expensive for home use
- Treatment protocols vary with limited standardization
- Requires multiple sessions for optimal results
- Effectiveness can vary based on individual factors and the specific wound type
Tips for Effective LLLT Treatment:
- Cleanliness is Key: Clean the wound thoroughly before treatment to optimize light penetration.
- Consistency Matters: Consistent treatments (2-3 times weekly) yield better results than sporadic application.
- Treatment Duration: Typical treatments range from 30 seconds to 5 minutes per area, depending on the device and protocol.
- Light Source Options: Both coherent (laser) and non-coherent (LED) light sources can be effective.
When to Consider LLLT:
LLLT is a valuable option for patients with chronic or acute wounds that are slow to heal. This includes individuals with:
- Surgical wounds
- Diabetic ulcers
- Pressure ulcers
- Burns
- Traumatic injuries
It's particularly relevant for elderly patients, those with compromised immune systems, and individuals seeking a non-invasive and effective way to accelerate skin healing. While LLLT equipment can be expensive for personal use, it is increasingly available in wound care clinics and physical therapy practices. Consulting with a healthcare professional experienced in LLLT is crucial to determine if this therapy is appropriate for your specific needs and to develop a personalized treatment plan.
7 Methods for Faster Skin Healing Comparison
| Remedy / Method | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Proper Wound Cleaning and Dressing | Moderate: Requires technique and regular care | Low: Basic materials like soap, saline, dressings | High: Accelerates healing by up to 50%, reduces infection and scarring | Everyday wounds needing infection control and faster healing | Well-researched, cost-effective, accessible, protects wound |
| Aloe Vera Gel | Low: Easy to apply, can be home-extracted | Low: Plant or commercial gel | Moderate: Reduces inflammation, soothes pain, speeds superficial healing | Minor burns, superficial cuts, natural healing preference | Natural, widely available, minimal side effects |
| Medical-Grade Honey | Moderate: Proper application needed | Moderate to high: Specialty honey and dressings | High: Strong antibacterial effect, promotes tissue regeneration | Chronic wounds, antibiotic-resistant infections | Potent antimicrobial, reduces odor, natural debridement |
| Zinc Supplementation | Low to moderate: Oral or topical use | Low: Supplements or dietary sources | Moderate: Enhances systemic healing, especially if deficient | Nutritional support, impaired healing due to deficiency | Addresses underlying deficiency, inexpensive, systemic effect |
| Growth Factor Therapies | High: Requires medical administration | High: Prescription products, handling, storage | Very High: Dramatically accelerates healing, especially chronic wounds | Chronic, difficult-to-heal wounds, diabetic ulcers | Cutting-edge, personalized, reduces scarring |
| Hyperbaric Oxygen Therapy (HBOT) | Very High: Specialized chamber and sessions | Very high: Expensive equipment and multiple sessions | Very High: Rapid healing of hypoxic and chronic wounds | Severe wounds with poor circulation, radiation injuries | FDA-approved, non-invasive, enhances multiple healing aspects |
| Low-Level Laser Therapy (LLLT) | Moderate to high: Equipment and repeated sessions | Moderate to high: Laser or LED devices | Moderate to high: Accelerates healing through cellular stimulation | Varied wound types, including infected wounds | Non-invasive, painless, synergistic with other treatments |
Taking Charge of Your Healing Journey
Understanding what helps skin heal quickly is crucial for anyone experiencing a wound, whether a minor scrape or a chronic condition. From proper wound cleaning and dressing to advanced therapies like growth factors and hyperbaric oxygen, the strategies discussed in this article provide a comprehensive overview of how to promote efficient healing. Key takeaways include the importance of maintaining a clean wound environment, the potential benefits of natural remedies like aloe vera and medical-grade honey, and the role of nutritional support with zinc. For more complex cases, exploring options like growth factor therapies, HBOT, and LLLT can significantly accelerate the healing process. Mastering these concepts empowers you to take an active role in your recovery and minimize potential complications. This knowledge is especially valuable for individuals managing chronic wounds, enabling them to improve their quality of life and regain their independence.
By prioritizing appropriate wound care, you not only address the immediate issue but also contribute to your overall well-being. Efficient wound healing minimizes scarring, reduces the risk of infection, and allows you to return to your normal activities sooner. For those seeking expert guidance and advanced wound care solutions, Rapid Wound Care offers specialized treatments designed to optimize healing and improve patient outcomes. These services can be conveniently provided in the comfort of your own home. If you’re ready to accelerate your healing journey and experience the benefits of comprehensive wound care, visit Rapid Wound Care today to learn more and schedule a consultation.

