Understanding Pressure Ulcer Risk
Pressure ulcers pose a serious threat to patients with limited mobility. This listicle provides a concise overview of 8 pressure ulcer assessment tools to aid in early identification and prevention. Learn about the Braden Scale, Norton Scale, Waterlow Score, PURPOSE T, PUSH Tool, Glamorgan Scale, Cubbin-Jackson Scale, and Qscale. Quickly compare their strengths and weaknesses to determine the most appropriate pressure ulcer assessment tool for your patients' needs. This information empowers healthcare providers to make informed decisions and improve patient care.
1. Braden Scale for Predicting Pressure Sore Risk
The Braden Scale is one of the most widely used and respected pressure ulcer assessment tools available for predicting pressure sore risk. Developed by Barbara Braden and Nancy Bergstrom in 1987, this tool provides a structured approach to evaluating a patient's vulnerability to developing pressure ulcers (also known as pressure sores or bedsores). It achieves this by assessing six key risk factors: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. This makes it a valuable tool for a range of individuals and institutions, including patients with chronic or acute wound conditions, primary care providers, long-term care facilities, wound care specialists, and even Medicare and insurance beneficiaries making coverage decisions.
Each of the six parameters within the Braden Scale is scored individually on a scale of 1 to 4, with the exception of friction/shear, which is scored from 1 to 3. Lower scores on each parameter indicate a higher level of risk for that specific factor. These individual scores are then summed to calculate a total score ranging from 6 to 23. A total score of 18 or less generally signifies that the patient is considered at risk for developing a pressure ulcer, with progressively lower scores correlating to increasingly higher risk levels. The Braden Scale's inclusion in this list of pressure ulcer assessment tools is warranted due to its widespread adoption, proven efficacy, and ease of use. For further information, you can learn more about Braden Scale for Predicting Pressure Sore Risk.
Features and Benefits:
- Comprehensive Risk Assessment: Evaluates six key risk factors, offering a holistic view of a patient's vulnerability.
- Clear Scoring System: Uses a numerical scoring system (6-23) that facilitates easy interpretation and risk stratification. Scores ≤18 identify at-risk individuals.
- Versatility: Can be used across diverse healthcare settings, including hospitals, nursing homes, home care, and long-term care facilities.
- Efficiency: Takes approximately 3-5 minutes to complete once the user is adequately trained.
- Cost-Effective: The Braden Scale is free to use in clinical practice, although proper citation is required.
Pros:
- Validated and Reliable: Extensively validated across multiple care settings and patient populations, demonstrating high reliability and predictive validity when used by trained professionals.
- Easy to Learn and Use: Simple to implement with minimal training required, making it accessible to a wide range of healthcare providers.
- Widely Accepted: Recognized as a standard of care for pressure ulcer risk assessment in many healthcare institutions.
Cons:
- Limitations in Specific Populations: May not be as effective in assessing risk in certain populations, such as critically ill patients and individuals with darker skin tones, where visual assessment of skin changes can be challenging.
- Subjectivity: Some degree of subjective interpretation is involved in scoring certain parameters, which can lead to interrater variability if not used consistently.
- Omission of Certain Risk Factors: Does not account for all potential risk factors, such as poor perfusion or the effects of certain medications.
- Limited Use in ICU: Its predictive ability in intensive care unit (ICU) patients may be limited due to the complex and rapidly changing conditions often present in this setting.
Implementation Tips:
- Proper Training: Ensure all staff using the Braden Scale receive appropriate training on its correct application and interpretation.
- Regular Reassessment: Conduct regular reassessments, particularly after changes in a patient's condition, to monitor risk and adjust interventions accordingly.
- Combine with Clinical Judgment: Use the Braden Scale in conjunction with clinical judgment and other assessment data to develop a comprehensive care plan.
- Documentation: Document Braden Scale scores and associated interventions in the patient's medical record.
The Braden Scale remains a crucial pressure ulcer assessment tool for identifying at-risk individuals and guiding preventative interventions. By understanding its features, benefits, and limitations, healthcare professionals can effectively utilize this tool to enhance patient care and reduce the incidence of pressure ulcers.
2. Norton Scale
The Norton Scale is a widely recognized pressure ulcer assessment tool, earning its place on this list due to its simplicity and long-standing history in clinical practice. Developed in 1962, it remains a popular choice, particularly for quick screening in various healthcare settings. This tool helps clinicians identify individuals at risk for developing pressure ulcers, enabling timely intervention and preventive measures. This makes it especially useful for patients with chronic or acute wound conditions, elderly patients, primary care providers, long-term care facilities, and anyone involved in managing patient care where pressure ulcer risk is a concern.
How the Norton Scale Works:
The Norton Scale assesses pressure ulcer risk based on five key parameters:
- Physical Condition: Assesses the patient's general physical health and well-being.
- Mental Condition: Evaluates the patient's mental state, including alertness and awareness.
- Activity: Measures the patient's level of activity and mobility.
- Mobility: Assesses the patient's ability to change and control body position.
- Incontinence: Considers the patient's level of continence for both bowel and bladder function.
Each parameter is scored on a scale of 1 to 4, with 4 representing the best possible condition and 1 indicating the worst. A total score is calculated by summing the individual scores for each parameter, resulting in a range from 5 to 20. A lower total score signifies a higher risk of pressure ulcer development. Scores of 14 or less are generally considered indicative of at-risk status.
Features and Benefits:
- Simplicity and Speed: The Norton Scale is quick to administer, typically taking only 2-3 minutes to complete. This makes it a practical tool for busy healthcare professionals.
- Ease of Use: The straightforward scoring system requires minimal training to implement correctly, making it accessible to a wide range of healthcare providers.
- Cost-Effective: There are no licensing fees associated with using the Norton Scale in clinical practice.
- Established Reliability: The scale has a long history of clinical use and has demonstrated reliability in various settings.
Pros:
- Simpler and faster to use than many other pressure ulcer assessment tools.
- Long history of clinical use and established reliability.
- No licensing fees required for clinical use.
- Effective for screening general adult populations.
Cons:
- Less comprehensive than newer pressure ulcer assessment tools like the Braden Scale.
- Does not include nutritional status as a risk factor, which is a known contributor to pressure ulcer development.
- Lower sensitivity and specificity compared to more comprehensive tools.
- Limited validation in diverse patient populations.
Implementation Tips:
- Conduct the assessment regularly, particularly for patients at higher risk.
- Use the Norton Scale in conjunction with clinical judgment and other relevant patient information.
- Document the Norton score and any interventions taken to address identified risks.
Comparison with Other Tools:
While the Norton Scale provides a quick and easy initial assessment, more comprehensive tools like the Braden Scale offer a more in-depth evaluation of risk factors, including sensory perception, moisture, nutrition, and friction/shear. If a patient scores low on the Norton Scale, consider using a more comprehensive tool like the Braden Scale for a more detailed assessment.
By understanding the features and limitations of the Norton Scale, healthcare professionals can effectively utilize this tool as part of a comprehensive pressure ulcer prevention strategy. This benefits patients, providers, long-term care facilities, and ultimately helps reduce the incidence of pressure ulcers.
3. Waterlow Score
The Waterlow Score, developed by Judy Waterlow in 1985, is a comprehensive pressure ulcer assessment tool widely used in the UK and parts of Europe. It stands out among pressure ulcer assessment tools due to its in-depth analysis of various risk factors contributing to pressure ulcer development. Unlike simpler tools that may focus solely on mobility, the Waterlow Score considers a broader picture, including build/weight, skin type, gender, age, continence, mobility, nutritional status, medication, and special risk factors such as tissue malnutrition, neurological deficits, and recent surgery/trauma. This makes it a valuable tool for predicting and preventing pressure ulcers in diverse patient populations. It's designed to be both a risk assessment and a guide for preventative measures and treatment strategies.
The Waterlow Score utilizes a numerical scoring system ranging from 1 to 64. A score of 10 or above signifies that the individual is "at risk" for developing a pressure ulcer. A score of 15+ indicates "high risk," while a score of 20+ designates "very high risk." Visual body maps are often incorporated into the assessment process, allowing healthcare professionals to document the location and severity of any existing pressure damage. The inclusion of special risk factors, such as the effects of certain medications (e.g., steroids) and recent surgical procedures, further enhances the tool's accuracy and clinical utility. This tool aims to give practitioners the information needed to not only assess risk but to also develop personalized prevention strategies. For instance, a patient with a high score due to immobility and poor nutrition might require a specialized mattress, a repositioning schedule, and dietary adjustments.
One of the key advantages of the Waterlow Score is its comprehensiveness. It offers a more detailed assessment than many other pressure ulcer assessment tools, especially regarding medication and surgical factors often overlooked by simpler tools. Its widespread use in UK and European healthcare systems testifies to its practical value and acceptance within the medical community. Furthermore, the Waterlow Score goes beyond simple risk stratification by providing guidance for preventative strategies tailored to the identified risks. You can learn more about Waterlow Score and its applications on various websites.
However, the Waterlow Score's complexity also presents certain challenges. It can be more time-consuming to complete compared to simpler scales, requiring more training for healthcare professionals to accurately interpret the scoring system. Some studies suggest that it may overestimate risk in specific populations, highlighting the importance of considering individual patient circumstances. While widely adopted in Europe, the Waterlow Score has seen less extensive validation in North American settings, which may limit its applicability in those regions. Currently, there's no specific pricing or technical requirement associated with the tool itself, as it's primarily a scoring system and methodology. It is often integrated into existing patient management systems or used through printed assessment forms. For healthcare practitioners working with elderly patients, particularly in long-term care facilities and communities, Medicare and Insurance beneficiaries, and those with chronic or acute wound conditions, the Waterlow Score, despite its complexities, offers valuable insight for proactive pressure ulcer prevention and management.
4. PURPOSE T (Pressure Ulcer Risk Primary Or Secondary Evaluation Tool)
PURPOSE T (Pressure Ulcer Risk Primary Or Secondary Evaluation Tool) stands out among pressure ulcer assessment tools for its innovative three-step approach, specifically designed to distinguish between patients requiring preventative measures and those already experiencing pressure damage. This makes it a valuable addition to any healthcare setting focused on comprehensive pressure ulcer management. Unlike traditional pressure ulcer assessment tools that primarily focus on risk prediction, PURPOSE T also addresses the needs of individuals with existing ulcers, guiding clinicians towards appropriate treatment strategies.
This tool, developed at the University of Leeds through rigorous research, begins with Step 1, screening for pressure ulcer history and analyzing a patient's independent movement. Step 2 delves into detailed risk factors, considering elements like mobility, nutrition, and skin condition. Finally, Step 3 utilizes a decision pathway to determine whether primary prevention (for those without ulcers) or secondary prevention/treatment (for those with existing pressure damage) is necessary.
PURPOSE T offers several key features that enhance its practical application:
- Structured Three-Step Approach: This ensures a comprehensive assessment, leaving no stone unturned.
- Color-Coded System: Risk levels are visualized through a color-coded system, making it easy for clinicians to quickly grasp a patient's status and prioritize care accordingly.
- Primary/Secondary Prevention Distinction: The key differentiator of PURPOSE T is its ability to explicitly identify patients with existing pressure ulcers, facilitating targeted intervention.
- Detailed Body Maps: Integrated body maps allow for meticulous documentation of skin status, helping track changes and monitor healing progress.
- Patient and Clinician Input: The tool's development benefited from direct feedback from both patients and clinicians, ensuring its practicality and relevance in real-world settings.
Why PURPOSE T Deserves Its Place in This List:
PURPOSE T addresses a crucial gap in many existing pressure ulcer assessment tools by recognizing the distinct needs of individuals with existing pressure damage. Its comprehensive three-step process, combined with the clear differentiation between primary and secondary prevention, offers a more nuanced and effective approach to pressure ulcer management. This, coupled with its evidence-based design, makes it a valuable tool for various healthcare professionals, including wound care specialists, primary care providers, and long-term care staff.
Pros:
- Evidence-based design: Built on a strong theoretical foundation with rigorous research backing.
- Accurate Identification: More accurately identifies patients with existing pressure damage compared to traditional scales.
- Clearer Decision Pathways: Provides more explicit guidance for clinical action, simplifying treatment decisions.
- Reduced Ceiling Effect: Mitigates the limitations of traditional scales that often struggle to differentiate between high-risk individuals.
Cons:
- Relative Newness: Being a relatively new tool, it has less long-term validation compared to more established assessments.
- Time Commitment: Takes slightly longer to complete (approximately 5-10 minutes) than simpler scales.
- Training Requirement: Requires specific training to ensure accurate implementation.
- Limited Availability: Currently, availability is primarily limited to the UK.
Implementation Tips:
- Seek out certified training programs to familiarize yourself with the tool's nuances.
- Utilize the color-coded system and body maps to efficiently document and track patient progress.
- Integrate PURPOSE T into existing wound care protocols for seamless implementation.
Pricing and Technical Requirements:
Information regarding pricing and specific technical requirements isn't readily available on the website. Contact the University of Leeds directly for further details.
Website: https://medhealth.leeds.ac.uk/info/423/skin/1738/purpose_t
This comprehensive pressure ulcer assessment tool empowers clinicians to move beyond basic risk prediction towards a more targeted and individualized approach to care, improving outcomes for patients with and without existing pressure ulcers. While the need for training and its relative newness are considerations, its strengths in accurate identification and clear decision pathways make PURPOSE T a valuable tool in the fight against pressure ulcers.
5. Pressure Ulcer Scale for Healing (PUSH)
The Pressure Ulcer Scale for Healing (PUSH) is a valuable tool for anyone involved in pressure ulcer management, including patients, caregivers, and healthcare professionals. Unlike pressure ulcer risk assessment tools, the PUSH tool focuses specifically on monitoring the healing progress of existing pressure ulcers. This makes it an essential part of any comprehensive pressure ulcer assessment toolkit. By objectively tracking wound changes, the PUSH tool facilitates evidence-based decision-making and improves the quality of pressure ulcer care.
This tool, developed by the National Pressure Ulcer Advisory Panel (NPIAP), deserves its place on this list because it provides a standardized, easy-to-use method for documenting wound healing. It’s particularly useful for long-term care facilities, wound care specialists, and other healthcare practitioners dealing with pressure ulcer patients. Medicare and insurance beneficiaries, as well as their families, can also benefit from understanding the PUSH tool as it provides a clear picture of treatment effectiveness.
How PUSH Works:
The PUSH tool assesses three key wound characteristics:
- Surface Area: Measured using a provided guide to ensure consistency.
- Exudate Amount: Evaluates the amount of drainage from the wound.
- Tissue Type: Assesses the appearance of the wound bed (e.g., granulation tissue, slough, necrotic tissue).
Each parameter is scored individually, and these scores are combined to generate a total PUSH score ranging from 0-17. A higher score indicates a more severe wound. By regularly assessing and recording the PUSH score, clinicians can monitor healing progress or identify any deterioration requiring care plan adjustments. The assessment typically takes only 2-4 minutes per wound.
Benefits of Using PUSH:
- Simple and Reliable: The PUSH tool is straightforward and easy to implement, even for those with limited wound care experience. Its simplicity ensures reliability and consistency in assessments.
- Objective Documentation: It provides a standardized way to document wound healing progress, facilitating clear communication among healthcare providers and enabling accurate tracking of treatment effectiveness.
- Serial Assessments: The PUSH tool is specifically designed for repeated assessments, making it ideal for monitoring healing over time.
- Validated Across Various Care Settings: The tool has been proven effective in various healthcare environments, from hospitals to home care settings.
- Free and Accessible: The PUSH tool, including downloadable forms and instructions, is freely available from the NPIAP website (https://npiap.com/page/PUSHTool). There are no technical requirements or software needed to use the tool.
Limitations of PUSH:
- Not a Risk Assessment Tool: It’s important to note that PUSH is not designed to assess the risk of developing pressure ulcers. It only monitors existing wounds.
- Single Wound Assessment: Each PUSH form is designed for assessing a single wound. Multiple wounds require multiple forms.
- Doesn't Capture Undermining or Tunneling: The PUSH tool doesn't specifically account for wound undermining or tunneling, which can be important aspects of wound assessment.
- Simplified Measurements: While the simplicity of PUSH is a strength, the simplified measurements may miss subtle changes in wound condition.
Implementation Tips:
- Training: Ensure all staff involved in wound care are trained on the proper use of the PUSH tool.
- Regular Assessments: Consistent, regular assessments are crucial for accurate monitoring of healing progress. Establish a clear schedule for PUSH assessments based on individual patient needs.
- Documentation: Maintain clear and accurate records of all PUSH scores to track changes over time.
- Communication: Use PUSH scores to communicate wound status and progress with the patient, their family, and other healthcare professionals.
The PUSH tool is a practical and valuable addition to any pressure ulcer assessment strategy, contributing to improved patient outcomes and more effective wound care. By focusing on objective measurement and tracking of wound healing, the PUSH tool empowers clinicians and patients alike to make informed decisions and optimize the healing process.
6. Glamorgan Scale
The Glamorgan Scale stands out among pressure ulcer assessment tools because it's specifically designed for pediatric patients aged 0-18 years. While many tools focus on adults, the Glamorgan Scale recognizes the unique physiological and developmental factors that influence pressure ulcer risk in children. This makes it a crucial tool for anyone involved in pediatric care, offering a more accurate risk assessment than adult-focused scales. This inclusion in our list of pressure ulcer assessment tools is vital for healthcare professionals working with young patients.
This tool evaluates 10 key risk factors, each assigned a weighted score:
- Mobility: Assessing the child's ability to move and reposition themselves.
- Equipment/Objects/Hard Surface Pressing or Rubbing on Skin: Considering the impact of medical devices, toys, or other objects.
- Significant Anemia: Evaluating the impact of reduced red blood cell count on oxygen delivery to tissues.
- Persistent Pyrexia (Fever): Recognizing the increased metabolic demands and potential skin breakdown associated with fever.
- Poor Peripheral Perfusion: Assessing circulation to the extremities, which can impact skin health.
- Inadequate Nutrition: Considering the role of proper nutrition in skin integrity and wound healing.
- Low Serum Albumin: Evaluating albumin levels, a marker of nutritional status.
- Incontinence: Recognizing the increased risk associated with moisture exposure.
- Weight Percentile: Considering the child's weight in relation to their age and development.
Total scores range from 0-42+, with the following risk stratification:
- 10+: At risk for developing a pressure ulcer.
- 15+: High risk for developing a pressure ulcer.
- 20+: Very high risk for developing a pressure ulcer.
Features and Benefits:
- Pediatric-Specific: Addresses the unique risk factors in children, offering higher sensitivity and specificity compared to adult scales.
- Comprehensive Assessment: Evaluates 10 pediatric-specific risk factors, including developmental considerations and common pressure points from medical equipment.
- Clear Risk Stratification: Provides clear cut-off scores for identifying patients at risk, enabling timely interventions.
- Validated in Multiple Settings: Proven effective in various pediatric environments, including NICU, PICU, and general pediatrics.
- Free to Use: No licensing fees for clinical use, making it accessible to all healthcare providers.
Pros:
- Higher sensitivity and specificity in pediatric populations compared to adult-focused pressure ulcer assessment tools.
- Validated in multiple pediatric settings.
- Addresses developmental and physiological factors unique to children.
- No cost for implementation.
Cons:
- Less widely implemented than adult scales like the Braden Scale.
- Fewer validation studies compared to some adult scales.
- Requires specific training for accurate pediatric assessment.
- Not suitable for adult populations.
Implementation Tips:
- Ensure staff receives adequate training on the proper use of the Glamorgan Scale and interpretation of scores.
- Integrate the scale into routine pediatric assessments, particularly for patients with limited mobility or other identified risk factors.
- Use the results to guide preventative interventions, such as repositioning, skin care, and nutritional support.
Website: https://www.nationalwoundcarestrategy.net/glamorgan-paediatric-pressure-ulcer-risk-assessment-scale/
The Glamorgan Scale is a valuable pressure ulcer assessment tool specifically designed for the pediatric population. Its use can help healthcare professionals accurately assess risk and implement appropriate interventions to prevent pressure ulcers in children.
7. Cubbin-Jackson Scale
The Cubbin-Jackson Scale stands out among pressure ulcer assessment tools due to its specialized focus on critical care patients. Unlike more general scales, it recognizes the unique challenges and heightened risks faced by individuals in intensive care units (ICUs). Developed in 1991, this tool provides a more nuanced and sensitive assessment for this vulnerable population. It delves into 10 key risk factors, including age, weight, general skin condition, mental condition, mobility, hemodynamic status, respiration, nutrition, incontinence, and hygiene. Each factor receives a score from 1 to 4, resulting in a total score ranging from 10 to 40. A score of 24 or less typically indicates a high risk of pressure ulcer development.
This scale's strength lies in its consideration of ICU-specific factors, such as hemodynamic instability (e.g., requiring vasopressors), respiratory compromise (e.g., mechanical ventilation), and the presence of multiple medical devices. These factors, often absent from general pressure ulcer assessment tools, significantly contribute to the risk profile of critically ill patients. The Cubbin-Jackson Scale acknowledges both intrinsic factors (like age and skin condition) and extrinsic factors (like hygiene and medical devices) that influence pressure ulcer development. This comprehensive approach makes it a valuable tool for healthcare professionals working in critical care settings.
Features:
- Specifically designed for critical care/ICU patients
- Evaluates 10 risk factors, including hemodynamic and respiratory status
- Scores range from 10-40, with ≤24 indicating high risk
- Accounts for factors like vasopressor use and mechanical ventilation
- Includes assessment of intrinsic and extrinsic risk factors
Pros:
- Higher sensitivity in critical care populations compared to general scales like the Braden Scale.
- Considers ICU-specific factors not included in general scales.
- Better predictive value for critically ill patients.
- Addresses both physiological and care-related factors.
Cons:
- More time-consuming to complete than simpler scales.
- Not widely validated outside critical care settings, limiting its applicability in other healthcare environments.
- Requires specific critical care knowledge for accurate scoring, potentially necessitating specialized training for staff.
- Less commonly implemented than more general tools like the Braden Scale, which may impact resource availability and familiarity among healthcare professionals.
Implementation Tips:
- Ensure staff involved in critical care are adequately trained on the proper use and interpretation of the Cubbin-Jackson Scale.
- Integrate the scale into the routine assessment protocols for all ICU patients.
- Regularly review and update pressure ulcer prevention strategies based on the assessed risk.
- Consider using the Cubbin-Jackson Scale in conjunction with other relevant assessments to provide a holistic view of the patient's condition.
Website: https://www.ncbi.nlm.nih.gov/books/NBK482358/
The Cubbin-Jackson Scale earns its place on this list of pressure ulcer assessment tools because of its targeted approach to critical care. While other tools may offer a broader scope, the Cubbin-Jackson Scale’s specialized focus provides a more accurate and relevant assessment for this high-risk population. Its ability to identify and quantify the unique risk factors present in the ICU setting makes it an invaluable tool for proactive pressure ulcer prevention and management in critical care. There is no cost associated with using the scale itself.
8. Qscale (Quebec Pressure Ulcer Risk Assessment Scale)
The Qscale (Quebec Pressure Ulcer Risk Assessment Scale) is a valuable addition to the arsenal of pressure ulcer assessment tools, particularly for healthcare professionals seeking a comprehensive and evidence-based approach. Developed in Canada, this relatively new tool aims to address limitations found in older scales by integrating the strengths of several existing instruments and incorporating the latest research on pressure ulcer development. This makes it a strong contender among pressure ulcer assessment tools available today.
The Qscale stands out for its detailed evaluation of 12 risk factors categorized into three key domains:
- Health Status: This domain assesses mental status, continence, nutritional status, and sensory perception, recognizing the impact of overall health on skin integrity.
- Mobility: Evaluating activity level, mobility, and the presence of friction/shear forces, this domain addresses the crucial role of movement and pressure on the development of ulcers.
- Skin Integrity: This domain directly examines the condition of the patient's skin and notes any history of previous pressure ulcers, providing crucial information about current vulnerability.
Each of the 12 risk factors is scored on a scale of 0-3, with higher scores indicating a greater risk of pressure ulcer development. The Qscale then generates both a total score and individual domain scores. This detailed breakdown is particularly useful for tailoring interventions. For example, a low mobility score might prompt interventions focused on repositioning and support surfaces, while a low nutrition score could trigger a referral to a dietitian.
Features and Benefits:
- Comprehensive Assessment: The Qscale's 12-factor assessment provides a thorough evaluation of a patient's risk, incorporating the latest evidence on pressure ulcer development.
- Targeted Interventions: The domain-specific scoring allows clinicians to pinpoint specific risk areas and develop targeted interventions, optimizing resource allocation and patient care.
- Multidisciplinary Approach: The Qscale was developed with input from a variety of healthcare professionals, reflecting a holistic understanding of pressure ulcer prevention.
- Accessibility: The tool is available in both English and French, broadening its applicability across different populations.
- Versatility: Designed for use in various healthcare settings, including acute care and long-term care facilities, the Qscale offers a consistent assessment approach across the continuum of care.
Pros:
- Comprehensive assessment incorporating the latest evidence.
- Domain scoring facilitates targeted interventions.
- Validated in various care settings.
- Developed with input from a multidisciplinary team.
Cons:
- Less widely implemented than established tools like the Braden Scale.
- Can require more time to complete compared to simpler scales.
- Limited long-term validation studies compared to older scales.
- Less internationally recognized than some established tools.
Implementation Tips:
- Familiarize yourself with the scoring guide and interpretation of domain and total scores.
- Incorporate the Qscale into routine patient assessments, particularly for those at high risk.
- Use the domain scores to guide the development of individualized care plans.
- Regularly reassess patients using the Qscale to monitor changes in risk and adjust interventions accordingly.
Pricing and Technical Requirements: While the Qscale itself is accessible through the provided website (https://www.preventingpressureinjuries.ca/qscale), there may be institutional costs associated with training and implementation. Check with your facility's wound care team or administration for details. No specialized technical equipment is required.
Although the Qscale is a newer tool and less recognized internationally than the Braden Scale, its comprehensive approach and focus on targeted interventions make it a valuable pressure ulcer assessment tool for clinicians striving to provide evidence-based, patient-centered care. It deserves a place in this list due to its potential to improve pressure ulcer prevention strategies, particularly through its comprehensive assessment and targeted intervention approach.
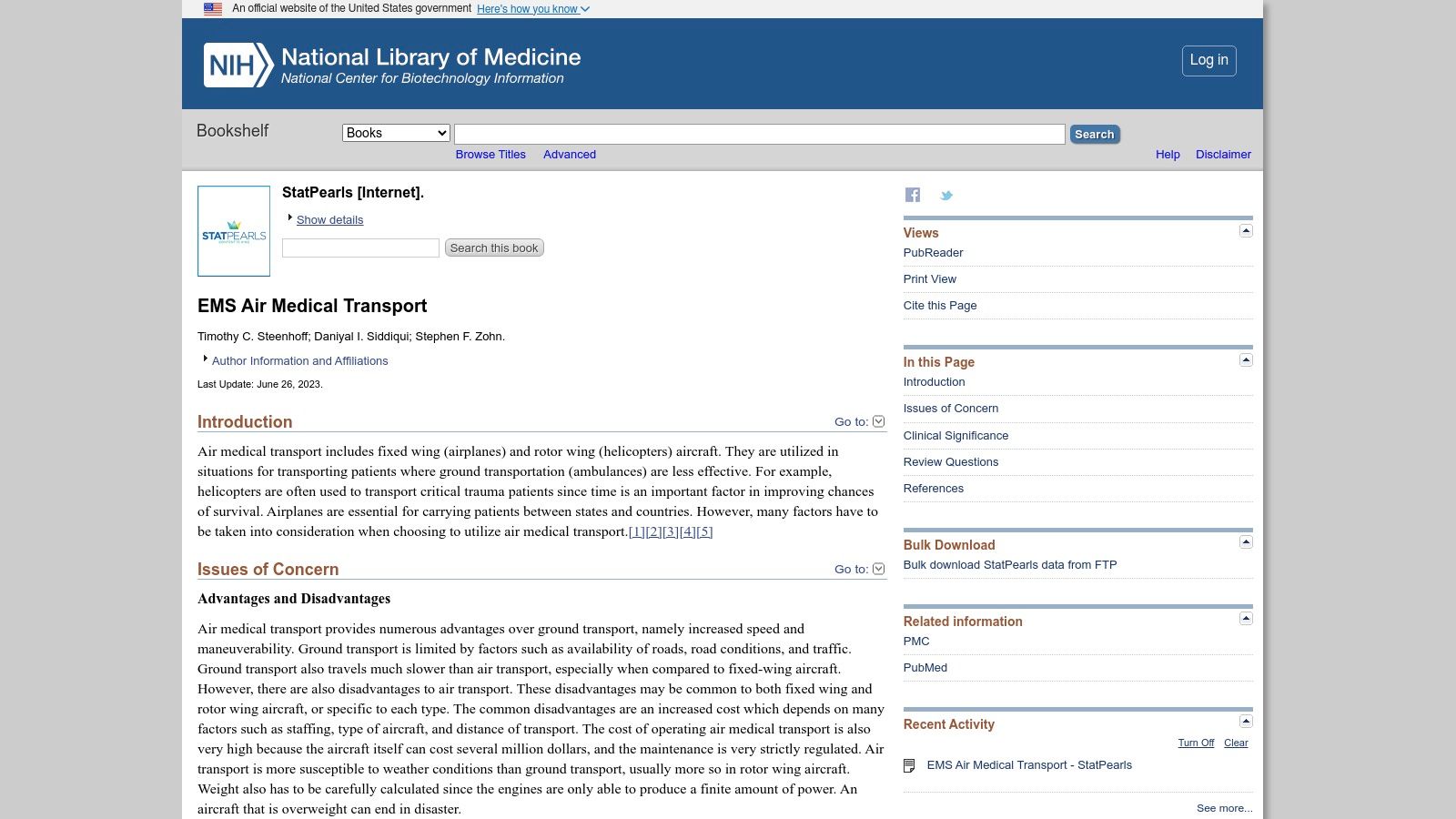
Pressure Ulcer Assessment Tools: Side-by-Side Comparison
| Assessment Tool | 🔄 Complexity | ⚡ Resource Requirements | 📊 Expected Outcomes | 💡 Ideal Use Cases | ⭐ Key Advantages |
|---|---|---|---|---|---|
| Braden Scale for Predicting Pressure Sore Risk | Moderate – 3-5 minutes with some subjectivity | Minimal – Basic training; free use | Risk categorization based on six parameters | Hospitals, nursing homes, home care | Extensively validated; high reliability; ease of use |
| Norton Scale | Low – 2-3 minutes; very simple process | Minimal – Requires very little training | Quick risk screening using five factors | General adult populations; screening in various settings | Long history in clinical use; simplicity; cost-free application |
| Waterlow Score | High – Comprehensive and time-consuming assessment | Moderate to high – Requires more training and detailed input | Detailed stratification with multiple risk categories | UK/European hospitals; patients with multiple risk factors | Comprehensive coverage; includes medication and surgical influences |
| PURPOSE T | Moderate to high – 5-10 minutes with structured steps | Moderate – Specific training required | Differentiates between prevention and treatment needs | Settings requiring clear decision pathways; UK settings | Evidence-based; distinguishes existing damage vs. risk only |
| Pressure Ulcer Scale for Healing (PUSH) | Low – 2-4 minutes per wound; simple to administer | Minimal – Basic training; forms available freely | Objective tracking of wound healing over time | Monitoring healing progress in clinical practice | Reliable; facilitates serial assessments; free accessibility |
| Glamorgan Scale | Moderate – Requires focused pediatric assessment | Moderate – Specialized pediatric training necessary | Accurate risk assessment tailored for pediatric patients | Pediatric settings (NICU, PICU, general pediatrics) | High sensitivity and specificity in children; developmentally informed |
| Cubbin-Jackson Scale | High – Detailed ICU-focused evaluation | High – Demands critical care expertise and careful evaluation | Risk prediction for critically ill with ICU-specific factors | Intensive care units; critical care settings | Sensitive for ICU patients; addresses hemodynamic and care-related factors |
| Qscale (Quebec Pressure Ulcer Risk Assessment Scale) | Moderate to high – In-depth, multidomain assessment | Moderate – Involves thorough data gathering and evaluation | Comprehensive risk scoring with domain-specific results | Acute and long-term care; multidisciplinary environments | Integrates multiple evidence-based scales; targeted intervention insights |
Choosing the Right Pressure Ulcer Assessment Tool
This article has explored a range of pressure ulcer assessment tools, from the widely used Braden Scale to more specialized tools like the PUSH tool for monitoring healing and the PURPOSE T for evaluating primary or secondary risk factors. Each tool offers unique advantages and considerations for different patient populations and care settings. Key takeaways include understanding the core components of each assessment, recognizing the specific risk factors they address (such as mobility, nutrition, and moisture), and appreciating the importance of regular reassessment.
Selecting the most appropriate pressure ulcer assessment tool depends heavily on your specific needs. Consider the complexity of the tool, the time required for administration, the patient's condition, and the resources available in your care setting. For instance, while the Braden Scale is a valuable tool for many, the Norton Scale might be more suitable for patients with cognitive impairments. If you're caring for an elderly loved one, providing holistic care is essential. For a comprehensive guide on providing compassionate care for the elderly, including physical, emotional, and practical support, check out this resource: Caregiving for the Elderly: Guide to Providing Compassionate Care.
Ultimately, consistent and accurate assessment, combined with timely interventions, is paramount in preventing and managing pressure ulcers. Early detection and proactive care can significantly improve patient outcomes and quality of life. For expert guidance and advanced treatment options in wound care, consider Rapid Wound Care. Their specialized team can assist with accurate pressure ulcer assessment, create personalized treatment plans, and provide the support you need to facilitate healing.

