The Wound Healing Symphony: Understanding the Recovery Process
Wound healing is a complex biological process, not just about closing the skin but restoring function and preventing complications. Understanding the distinct phases of wound healing is crucial for both medical professionals and patients. This improved understanding has led to significant advances in treatment, moving beyond simple bandages to therapies targeting specific phases.
The Four Key Movements in Wound Healing
The wound healing process is typically divided into four overlapping stages: hemostasis, inflammation, proliferation, and remodeling. Although distinct, these phases interact and transition smoothly, creating a continuous, dynamic process. Imagine these phases as separate movements within a musical composition, each contributing to the overall masterpiece of healing.
-
Hemostasis: The initial phase, hemostasis, stops the bleeding. Much like a conductor starting the orchestra, this phase sets the stage for healing.
-
Inflammation: The inflammation phase cleans the wound and prepares it for repair. Essential for removing debris and bacteria, this phase is like the percussion section, creating a powerful yet controlled response.
-
Proliferation: The proliferation phase focuses on rebuilding new tissue. Similar to the string section building the melody, this stage sees new cells and blood vessels forming to fill the wound.
-
Remodeling: The final phase, remodeling, strengthens and refines the newly formed tissue. This can be a long-term process lasting months or even years, like the lingering resonance of the symphony's final notes.
Why Understanding the Phases Matters
Recognizing these phases allows clinicians to implement targeted interventions for optimal results. For instance, during the inflammatory phase, interventions might focus on managing swelling and infection prevention. Understanding the phases also empowers patients to actively participate in their recovery. They can recognize healthy healing signs and seek timely intervention if needed.
This knowledge can significantly impact healing, leading to quicker recovery times and fewer complications. The phases of wound healing aren't merely a biological sequence; they're a roadmap to effective treatment and optimal recovery.
Hemostasis: The Critical First Response to Injury
Imagine nicking your finger while preparing dinner. Almost immediately, you see blood. This is where hemostasis, your body's natural "first aid" system, kicks in. This initial phase of wound healing, lasting from minutes to hours, sets the stage for recovery. It's a complex process designed to stop bleeding and pave the way for tissue repair.
Vasoconstriction: Narrowing the Vessels
The first step in hemostasis is vasoconstriction, the narrowing of your blood vessels. This reaction, similar to pinching a leaking hose, reduces blood flow to the injured area. This buys precious time for the next steps to take effect, preventing significant blood loss.
Platelet Aggregation: Forming the Plug
Next, platelets, small circulating cells, rush to the injury site. They stick together, forming a platelet plug – much like a temporary patch on a hose. This plug further slows blood flow and provides a base for the final step: coagulation. Wound healing progresses through four phases: hemostasis, inflammation, proliferation, and remodeling. This approximately two-day hemostasis phase is critical for halting bleeding and creating a foundation for further healing. Learn more: The Four Stages of Wound Healing
Coagulation: Building the Clot
Finally, coagulation transforms the temporary platelet plug into a stable blood clot. This involves a series of reactions with proteins called clotting factors, which create fibrin. Fibrin acts like a net, strengthening the platelet plug and forming a solid barrier against further bleeding. This clot not only stops blood loss but also provides a framework for the next phase of healing: inflammation.
The Hemostasis Timeline: A Visual Representation
The timeline below illustrates the sequence of events during hemostasis, from the initial injury to the formation of a stable clot.
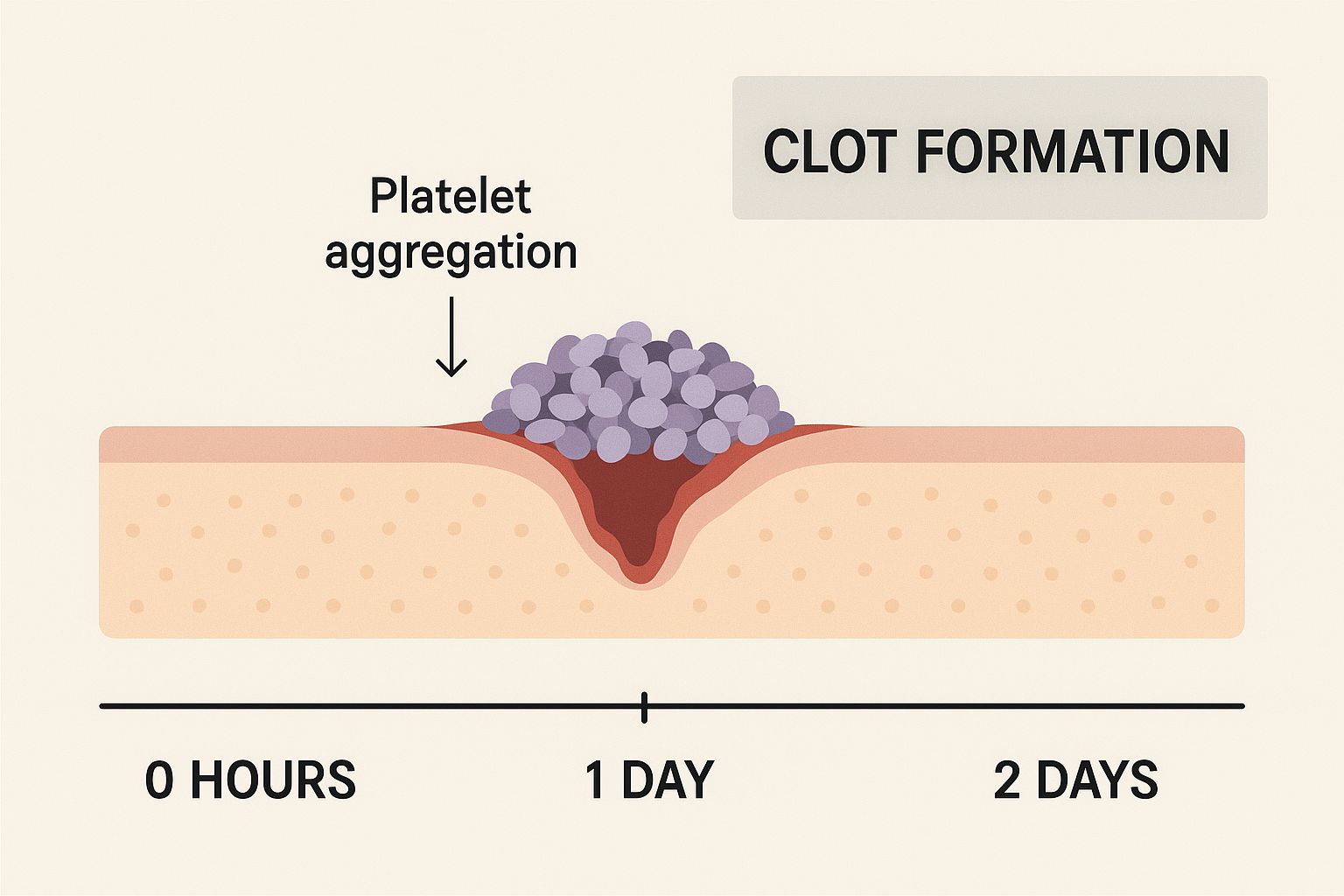
The timeline clearly shows how rapidly the body responds to injury, progressing from the initial break in the skin to a fully formed clot in a matter of hours. This rapid response is essential for minimizing blood loss and preparing the wound for the next stages of healing.
- Injury: The skin is broken, and bleeding begins. (0 seconds)
- Vasoconstriction: Blood vessels constrict to limit blood flow. (Seconds to minutes)
- Platelet Aggregation: Platelets adhere to the injury site and form a plug. (Minutes)
- Coagulation Cascade: Clotting factors activate, forming fibrin. (Minutes to hours)
- Stable Clot Formation: A stable clot forms, stopping bleeding and providing a framework for healing. (Hours)
The quick progression from injury to stable clot highlights the efficiency of hemostasis. This prompt action is crucial for effective wound management. Problems with this process, as seen in conditions like hemophilia, can cause uncontrolled bleeding and require medical attention. Understanding normal hemostasis is key for identifying when intervention is necessary.
Inflammation: The Double-Edged Sword of Healing
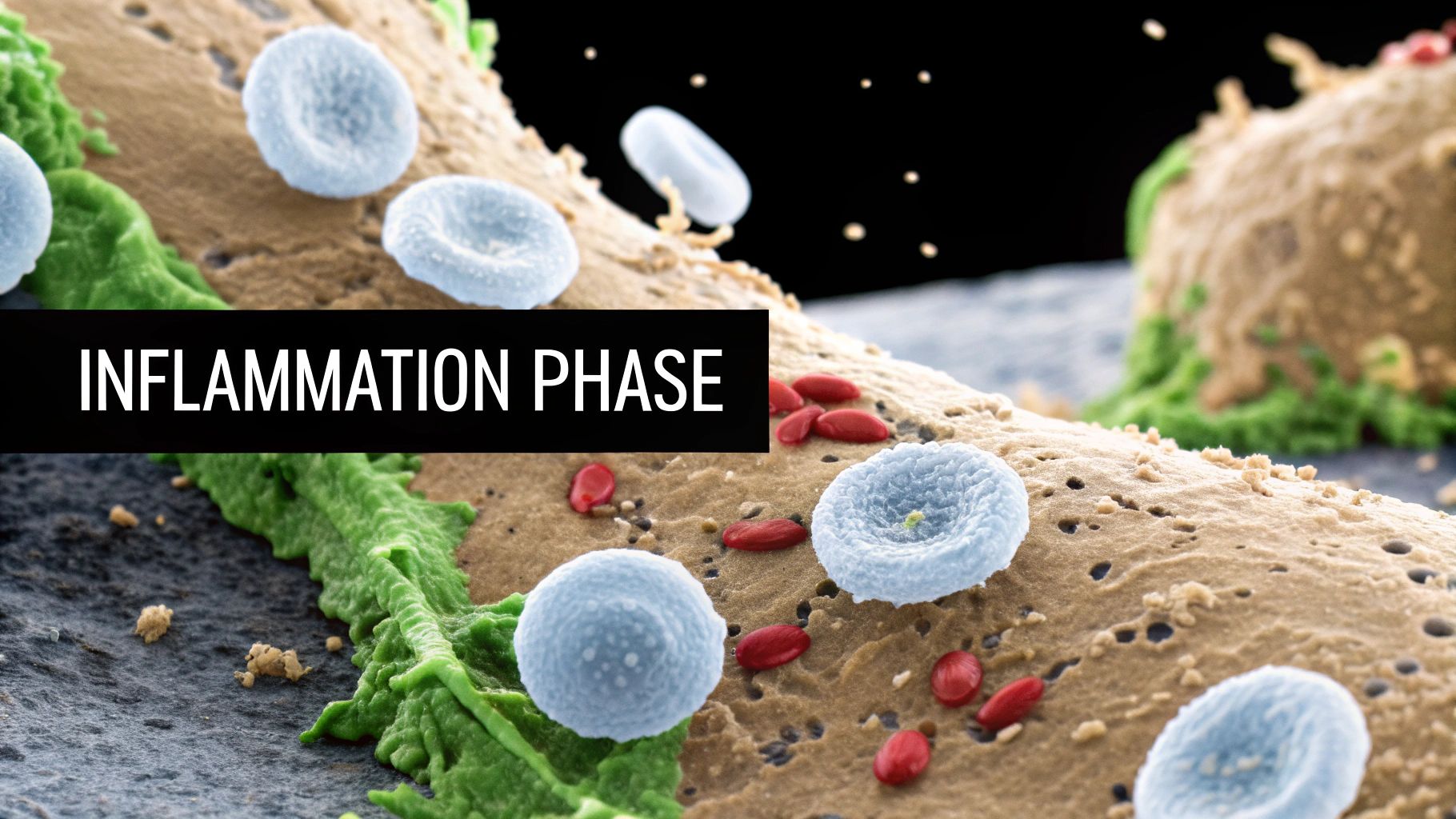
Following hemostasis, the next phase of wound healing is inflammation. Characterized by redness, heat, swelling, and pain, inflammation is a crucial part of the healing process, lasting from 2 to 14 days. This phase acts as the body's clean-up crew, preparing the wound bed for the important work of tissue regeneration. But uncontrolled or prolonged inflammation can become detrimental, hindering healing rather than promoting it.
The Purpose of Inflammation
Inflammation isn't simply about discomfort. It's a complex and carefully orchestrated series of events designed to clear debris and fight infection. This preparation is essential for the subsequent phases of wound healing to proceed effectively. This orchestrated response is driven by specialized cells that arrive at the wound site to carry out their specific functions.
Key Players in the Inflammatory Response
The inflammatory response involves a coordinated effort from several types of cells:
-
Neutrophils: These cells are the first responders, arriving early to engulf bacteria and debris through a process called phagocytosis. They are essential for clearing the initial damage.
-
Macrophages: Arriving a bit later, macrophages continue the cleaning process started by the neutrophils. They also release growth factors that stimulate tissue repair, setting the stage for the next phase of healing.
-
Lymphocytes: These cells play a vital role in the immune response, targeting any remaining pathogens and preventing infection. They help ensure a safe environment for healing to progress.
The Inflammatory Timeline
The inflammatory process unfolds in a specific sequence of events:
-
Vasodilation: Blood vessels widen, increasing blood flow to the injured area. This increased blood flow brings oxygen and nutrients necessary for healing and causes the characteristic redness and warmth.
-
Increased Permeability: Blood vessels become more permeable, allowing immune cells and fluid to enter the wound site. This influx of cells and fluid leads to swelling and can cause pain.
-
Chemotaxis: Chemical signals act as messengers, attracting immune cells to the wound area and guiding them to the precise location of the injury.
-
Phagocytosis: Neutrophils and macrophages engulf bacteria and debris, effectively cleaning the wound and preparing it for repair.
To better understand this critical phase, let's examine the signs, purpose, and key players involved in the inflammatory response. The following table summarizes the key aspects of this process.
| Sign/Symptom | Biological Purpose | Key Cellular Components | Timeline |
|---|---|---|---|
| Redness | Increased blood flow to deliver oxygen and nutrients | Vasodilation mediated by histamine and other mediators | Immediate – several days |
| Heat | Increased blood flow and metabolic activity | Vasodilation | Immediate – several days |
| Swelling | Influx of fluid and immune cells to the injured area | Increased vascular permeability | Hours – days |
| Pain | Stimulation of nerve endings by inflammatory mediators | Prostaglandins, bradykinin | Hours – days |
| Loss of Function | Protective mechanism to limit further injury | Swelling, pain | Variable |
This table highlights the interconnectedness of the signs and symptoms of inflammation and their underlying biological purposes. Understanding these connections helps appreciate the complexity of the inflammatory process.
The Delicate Balance: Acute vs. Chronic Inflammation
While essential for healing, inflammation must be carefully regulated. Acute inflammation is the normal, healthy response to injury, playing a vital role in tissue repair. However, if inflammation persists for too long or becomes excessive, it can transform into chronic inflammation. Chronic inflammation can damage healthy tissue and significantly delay the healing process.
Recognizing Problematic Inflammation
Prolonged inflammation can manifest in several ways:
- Excessive swelling and pain that doesn't subside
- Increased redness and heat around the wound
- Delayed healing or worsening of the wound
- Systemic symptoms like fever or chills
These signs indicate that inflammation has become counterproductive and requires intervention. Healthcare professionals can assess and manage these situations, implementing strategies to bring inflammation back under control and promote healthy healing. Addressing chronic inflammation requires careful evaluation and an individualized treatment plan. Recognizing the phases of wound healing allows for targeted interventions, optimizing the body's natural ability to repair itself.
Proliferation: The Rebuilding Revolution in Wound Healing
After the initial inflammation subsides, the wound enters the proliferation phase. This is a period of intense rebuilding and regeneration, typically lasting from days 2-21 post-injury. The wound transitions from damage control to repair, much like a construction site bustling with activity. This phase involves three key, simultaneous processes: angiogenesis, collagen deposition, and epithelialization.
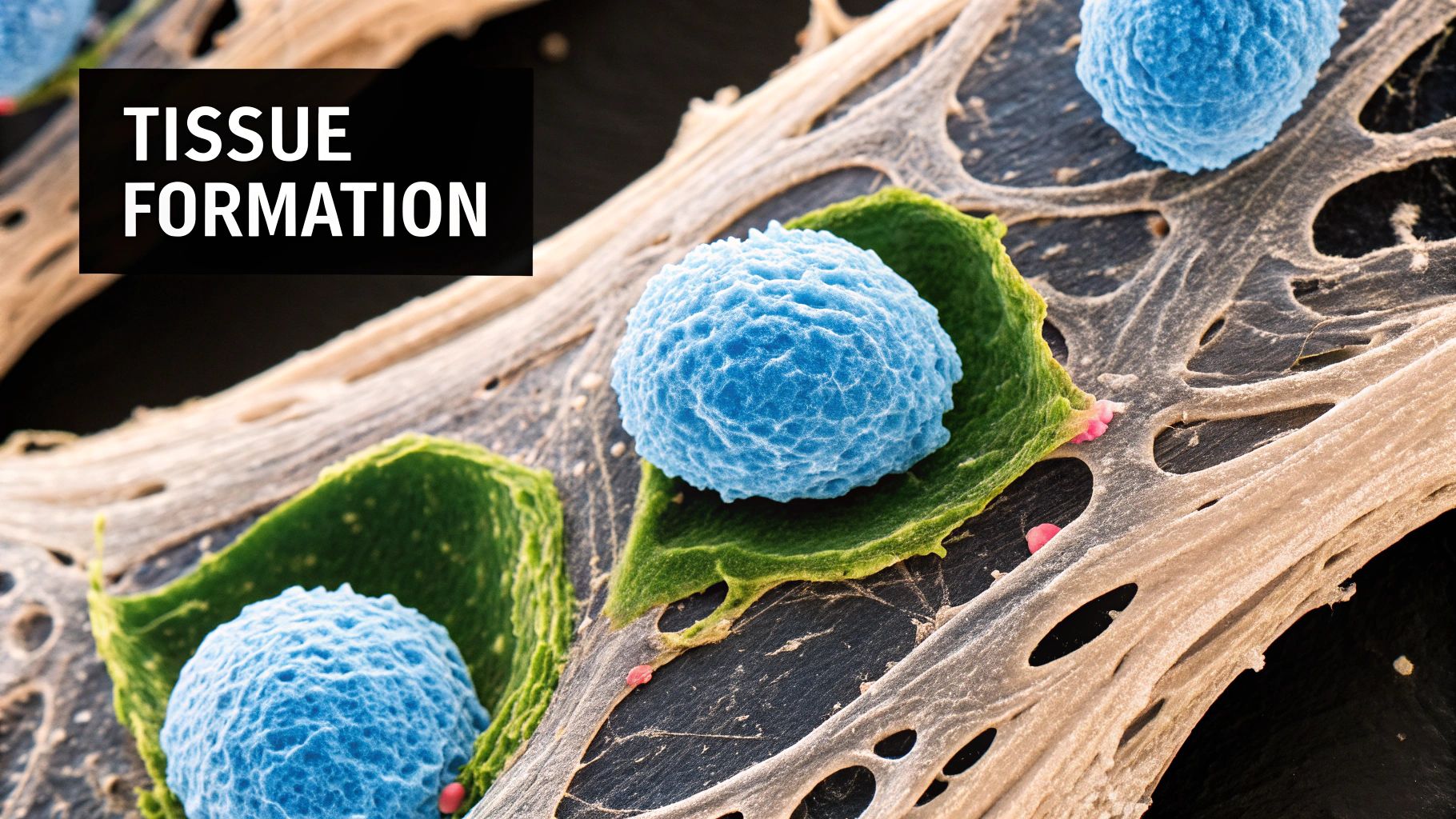
Angiogenesis: Building New Blood Supply
Angiogenesis is the formation of new blood vessels. These vessels are essential, delivering oxygen and nutrients to the regenerating tissue. They act like roads to a new city, ensuring the wound receives the necessary resources to rebuild. This process is driven by endothelial cells, which sprout from existing vessels and extend into the wound bed, creating a new network. Consider supporting your body with natural approaches like those found at The TN Hemp Company during the inflammation phase.
Collagen Deposition: Laying the Foundation
Collagen is a crucial structural protein that provides strength and support to the wound. During proliferation, fibroblasts synthesize and deposit new collagen. This is similar to laying bricks to build a wall, creating the structural framework for new tissue. The initial collagen, type III collagen, is less organized and weaker. This initial scaffold is critical for later remodeling stages, where it's replaced by the stronger, more organized type I collagen.
Epithelialization: Restoring the Protective Barrier
Epithelialization restores the skin's outer layer, the epithelium, which acts as a protective barrier against infection and dehydration. Specialized skin cells called keratinocytes migrate from the wound edges and proliferate, covering the wound surface like a new roof. This process is essential for restoring the wound's integrity.
Granulation Tissue: The Living Scaffold
These three processes contribute to forming granulation tissue. This bumpy, red tissue is a sign of healthy proliferation and acts as a living scaffold for further tissue growth. The red color comes from the new blood vessels, indicating a well-perfused wound bed. It's a sign of active healing, not a complication.
Recognizing Healthy Proliferation
Recognizing healthy proliferation is crucial for appropriate wound management. Here are some key indicators:
- Presence of granulation tissue: Look for the bumpy, red appearance.
- Wound contraction: The wound edges will start to pull together.
- Decreased exudate: There will be less fluid drainage from the wound.
However, persistent pain, excessive inflammation, or a lack of granulation tissue may indicate a problem requiring further evaluation by a healthcare professional. Understanding these phases allows for appropriate intervention and optimal management.
Modern Wound Care and Proliferation
Modern wound care technologies often focus on this phase. They aim to optimize conditions for angiogenesis, collagen deposition, and epithelialization. This targeted approach can significantly accelerate healing and improve patient outcomes.
Remodeling: The Art of Tissue Refinement and Strength
The remodeling phase is the final stage in the phases of wound healing. It showcases the body's remarkable ability to repair and refine injured tissue. This phase, spanning months or even years, strengthens new tissue and enhances its overall appearance. Even after a wound seems closed, significant changes continue beneath the surface.
Collagen Transformation: From Scaffold to Fortress
Initially, a wound is filled with type III collagen. This is a rapidly produced but relatively weak structural protein, acting as a temporary scaffold. During remodeling, this type III collagen is gradually replaced by type I collagen. Type I collagen is stronger, more organized, and provides long-term stability. This crucial transformation restores the tissue's tensile strength. Over time, the refined collagen structure can regain up to 80% of the original tissue's strength.
Scar Evolution: From Red to Fade
A fresh scar often appears red and raised because of increased blood flow and collagen production. As remodeling progresses, blood supply diminishes, and collagen fibers reorganize. This causes the scar to gradually fade and flatten. This visible change reflects the ongoing maturation and strengthening of the underlying tissue.
The Role of Mechanical Forces
Mechanical forces are key to proper collagen alignment. Everyday movements place gentle stresses and strains on the healing tissue. This guides collagen fibers into a more organized and functional arrangement, crucial for withstanding future stress. This highlights the importance of appropriate movement and rehabilitation during wound healing. These forces essentially sculpt the new tissue for optimal function.
Minimizing Scarring: Working With Your Body
Several strategies can help minimize scarring during the remodeling phase:
- Proper Tension Management: Reducing tension on the wound edges, through proper closure and positioning, minimizes scar tissue formation.
- Silicone Therapy: Silicone sheets or gels create a hydrated environment that can soften and flatten scars, improving their appearance.
- Other Interventions: Other methods, such as massage and pressure garments, may also contribute to scar reduction. These interventions work with the body's natural remodeling processes to refine the healed tissue for a better aesthetic outcome.
The remodeling phase is a long-term process of tissue refinement. It's a silent but vital process of cellular activity continuing long after the visible wound is healed. By understanding this complex process and supporting the body's natural mechanisms, we can promote optimal healing and minimize the long-term impact of injury. At Rapid Wound Care, our specialists understand these nuances. We utilize evidence-based approaches throughout all phases of wound healing to achieve the best possible outcomes for our patients. Learn more about our comprehensive wound care services at Rapid Wound Care.
Beyond Biology: What Makes or Breaks Your Healing Journey
The human body's remarkable ability to heal is a complex process, far more intricate than simply progressing through the four standard phases of wound healing. Why do seemingly identical wounds heal without a hitch in some individuals, yet present significant challenges for others? The answer lies in a complex interplay of factors that extend beyond basic biology. These factors influence every stage of healing, from the smallest cellular level to systemic processes throughout the entire body.
Individual Healing Environments: A Complex Equation
Each individual presents a unique healing environment, a complex landscape where various factors converge. Age, nutrition, oxygenation, infection status, medications, and underlying health conditions all play crucial roles. For instance, a younger person with a healthy diet and robust circulation may heal quickly. Conversely, an older individual with diabetes could experience significant delays. This highlights the critical importance of personalized wound care that addresses each patient's unique circumstances.
The Challenge of Chronic Wounds
Chronic wounds, such as diabetic ulcers, pressure injuries, and venous stasis ulcers, present unique obstacles to the healing process. In these cases, the normal phases of wound healing are often disrupted, leading to prolonged healing times and a heightened risk of complications. These wounds frequently stall in the inflammatory phase, creating a frustrating cycle of tissue damage and delayed repair.
Statistically, wound healing, particularly chronic wounds that fail to heal within four to six weeks, is a significant global concern. Approximately 5% of the population in developed countries suffers from chronic wounds, often stemming from conditions like diabetes, venous insufficiency, or arterial disease. The global wound care market reached $24.8 billion in 2020 and is projected to grow further with the aging population and rising rates of obesity and diabetes. More detailed statistics can be found here.
Addressing Unique Patient Challenges
Different patient populations face distinct challenges in the wound healing process. Individuals with diabetes, for example, often have impaired circulation and reduced immune function, both of which can hinder healing. Patients with venous insufficiency may experience swelling and poor blood flow to the lower extremities, complicating wound healing in those areas. These distinct challenges emphasize the need for specialized approaches tailored to each patient's specific needs and underlying conditions.
To better illustrate these factors, let's examine a comparison table:
Comparison of Factors Affecting Wound Healing
This table compares various local and systemic factors that can either promote or impair the wound healing process across all phases.
| Factor | Positive Impact | Negative Impact | Mitigation Strategies |
|---|---|---|---|
| Age | Younger age generally associated with faster healing | Older age can slow down healing due to decreased cell turnover | Optimize nutrition, manage comorbidities, promote mobility |
| Nutrition | Adequate protein, vitamins (A, C, E), and minerals (zinc, copper) support tissue repair and immune function | Deficiencies impair collagen synthesis, immune response, and overall healing | Dietary supplements, nutritional counseling |
| Oxygenation | Adequate oxygen supply is crucial for cell metabolism and collagen synthesis | Hypoxia impairs fibroblast function and angiogenesis | Supplemental oxygen, hyperbaric oxygen therapy, address underlying respiratory issues |
| Infection | A controlled initial inflammatory response is essential for clearing debris | Persistent infection prolongs inflammation and hinders tissue repair | Wound debridement, antimicrobial dressings, systemic antibiotics |
| Medications | Some medications (e.g., steroids) can be used to manage inflammation and pain | Certain medications (e.g., immunosuppressants, chemotherapy) can impair healing | Careful medication management, dose adjustments |
| Comorbidities | Well-managed chronic conditions contribute to overall health | Diabetes, vascular disease, and autoimmune disorders can significantly impair healing | Optimize management of underlying conditions |
This table highlights the complex interplay of factors influencing wound healing and underscores the necessity for a comprehensive approach to patient care. Addressing these factors individually and collectively can significantly improve healing outcomes.
Practical Strategies for Optimized Healing
Understanding these factors allows healthcare professionals to implement strategies to optimize healing and reduce complications. Here are a few key strategies:
- Nutrition: Ensuring adequate intake of protein, vitamins, and minerals supports tissue repair and strengthens immune function.
- Infection Control: Promptly addressing infections prevents further tissue damage and actively promotes healing.
- Oxygenation: Maintaining adequate oxygen levels is vital for cell function and the regeneration of new tissue.
- Medication Management: Certain medications can impair healing, requiring careful monitoring and potential adjustment.
By understanding and addressing these factors, patients and clinicians can work together to achieve optimal healing outcomes. At Rapid Wound Care, we employ evidence-based strategies and offer a personalized approach to care, addressing the unique needs of each patient throughout all phases of wound healing. Visit our website to learn more.
Leading-Edge Approaches to Supporting Each Healing Phase
The science of wound care has significantly advanced, moving beyond simply covering a wound to actively supporting each phase of the healing process. This means treatment plans are now strategically designed to optimize the body's natural healing cascade. This section explores some of the most effective, evidence-based interventions available today.
Hemostasis: Jumpstarting the Healing Process
The initial phase, hemostasis, focuses on stopping bleeding. Advanced hemostatic agents play a crucial role in quickly controlling bleeding, particularly in traumatic injuries. These specialized products work by promoting rapid clot formation, essentially accelerating the body's natural response. This quick action is crucial for minimizing blood loss and preparing for subsequent healing phases. For example, some agents use chitosan, a natural polymer derived from shellfish, to promote platelet aggregation and fibrin formation.
Inflammation: Modulating the Inflammatory Response
Inflammation, while essential for cleaning the wound, requires careful management. Excessive or prolonged inflammation can be detrimental. Interventions aim to modulate the inflammatory response, ensuring it's effective but not overwhelming. This can involve using advanced dressings that absorb excess exudate and create a moist wound environment. Optimizing your gut health can also significantly impact wound healing. To learn more about supporting this crucial ecosystem, read about how to heal your gut. Topical treatments containing anti-inflammatory agents can also help control local inflammation.
Proliferation: Accelerating Tissue Regeneration
The proliferation phase centers on rebuilding new tissue. Modern wound care uses advanced therapies to accelerate this process. Growth factor therapy, for instance, uses naturally occurring proteins to stimulate cell growth and blood vessel formation. This can significantly speed up the formation of granulation tissue and wound closure. Another key intervention is negative pressure wound therapy (NPWT). NPWT uses a controlled vacuum to remove excess fluid, reduce edema, and promote blood flow to the wound bed, creating an ideal environment for tissue regeneration.
Remodeling: Refining and Strengthening Healed Tissue
The final remodeling phase focuses on strengthening and refining the healed tissue. Interventions during this phase concentrate on optimizing scar formation and improving the overall aesthetic outcome. Silicone therapy, for example, uses silicone sheets or gels to hydrate and soften scar tissue, minimizing its appearance. Other techniques, such as massage and pressure garments, can further enhance scar remodeling by influencing collagen fiber alignment and reducing tension on the wound.
Personalized Wound Care: A Multidisciplinary Approach
Modern wound care recognizes the importance of personalized treatment. Skilled practitioners assess the wound and consider patient-specific factors like age, underlying health conditions, and nutritional status when developing a treatment plan. This individualized approach acknowledges that a "one-size-fits-all" method is rarely effective.
Multidisciplinary Wound Care Teams
Complex wounds often require a multidisciplinary approach. This involves a team of healthcare professionals, including physicians, nurses, physical therapists, and dietitians, working together to address all aspects of patient care. This collaborative strategy ensures all potential barriers to healing are identified and addressed, leading to improved patient outcomes. This collaborative effort can involve nutritional support, pain management, and addressing underlying medical conditions that may be impacting healing.
For comprehensive wound care services that utilize these advanced approaches, consider Rapid Wound Care. We offer personalized treatment plans and a multidisciplinary team to optimize healing and improve overall well-being.

