The Evolution of Wound Care: From Hospital to Home
Healthcare is constantly changing, and wound care is leading the way. Traditionally, treating a wound meant numerous trips to a hospital or clinic, disrupting lives and potentially increasing infection risk. However, in-home wound care services offer a convenient and often more effective path to healing. This shift emphasizes patient-centered care, prioritizing comfort and personalized treatment.
The Growing Need for In-Home Wound Care
The move towards home-based care isn't just about convenience; it's driven by a real need. Chronic wounds, such as diabetic foot ulcers and pressure injuries, require constant care. In-home wound care provides consistent treatment in a familiar setting, improving patient commitment and results. Post-surgical wounds also benefit from focused attention and reduced infection risk with in-home care. This personalized approach allows healthcare providers to customize treatment plans to individual needs and lifestyles.
The global wound care market, including in-home services, is booming. In 2024, the market reached USD 23.13 billion, fueled by the demand for surgical and chronic wound care. This growth is partly due to an aging population, with projections estimating 1 in 6 people will be 60 or older by 2030. This demographic shift highlights the growing need for accessible and affordable in-home wound care. Learn more about the growing wound care market
Benefits of Healing at Home
In-home wound care offers significant advantages. Healing in a familiar, comfortable space reduces stress and improves well-being, positively impacting recovery. Patients are more likely to follow treatment plans and achieve better results. In-home care can also be more affordable than frequent hospital visits, easing the financial strain on patients and the healthcare system.
From Traditional Methods to Modern Technology
In-home care doesn't mean sacrificing quality. Skilled nurses bring their expertise to the patient's home, using traditional and advanced techniques. This includes specialized dressings, cleaning methods, and technologies like negative pressure wound therapy. This combined approach delivers comprehensive care tailored to individual needs in the comfort of home.
Why Home Healing Works: The Benefits You Can't Ignore
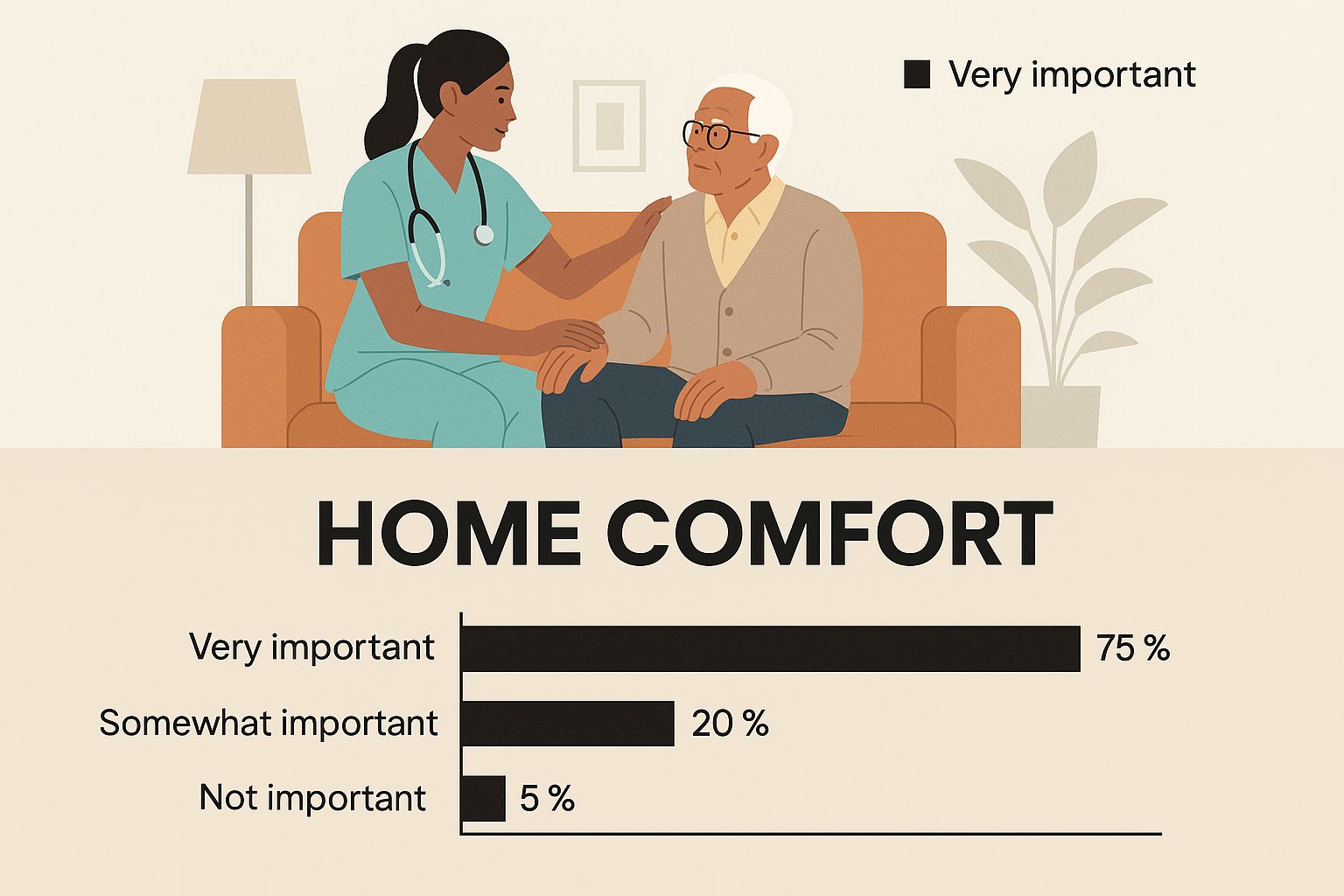
This infographic showcases the comforting environment of home, where a nurse provides personalized wound care to an elderly patient. The image highlights the relaxed and familiar atmosphere that home-based care offers. This setting promotes a sense of calm and well-being, essential for healing.
Healing at home isn't simply about convenience; it's about creating an environment conducive to recovery. In-home wound care services offer personalized care plans tailored to your living space and daily routines. This personalized approach significantly improves treatment adherence and overall patient outcomes.
Psychological Comfort: A Healing Advantage
The familiar surroundings of home offer psychological benefits that greatly influence the healing process. Stress levels often decrease in the comfort of one's own home, unlike in clinical settings. For instance, patients can maintain their routines and social connections, minimizing disruptions and promoting a sense of normalcy. This positive mindset contributes to faster healing and improved overall well-being.
Reduced Costs, Improved Outcomes
Beyond comfort, in-home wound care offers significant cost savings. These services reduce hospital readmissions and emergency room visits, lowering healthcare expenses for both individuals and the healthcare system. The consistent monitoring provided at home also leads to earlier detection of complications, preventing more serious issues.
To illustrate the growing need, the United States plays a major role in the global wound care market. By 2025, the U.S. is projected to account for over 45% of global wound care product demand. This underscores the increasing demand for in-home wound care services within the country, driven by the availability of advanced technologies and the rising need for home healthcare. Learn more about the future of wound care here.
To help you better understand the differences between hospital and in-home care, let's take a closer look at a comparison table. This table highlights key aspects of receiving wound care in different settings, focusing on the patient experience, cost, and overall outcomes.
| Aspect | Hospital-Based Care | In-Home Wound Care Services |
|---|---|---|
| Environment | Clinical, unfamiliar | Comfortable, familiar |
| Cost | Typically higher due to facility fees | Generally lower |
| Psychological Impact | Can be stressful, disruptive to routines | Reduces stress, maintains normalcy |
| Personalization | Standardized protocols | Individualized care plans |
| Convenience | Requires travel to appointments | Care delivered at home |
| Monitoring | Periodic check-ups | Consistent monitoring |
| Complication Detection | May be delayed | Earlier detection |
As this table illustrates, in-home wound care offers distinct advantages in terms of cost, comfort, and personalized attention. These factors contribute significantly to improved patient outcomes and overall satisfaction.
Expanding Options for Home Care
As wound care continues to evolve, understanding the various in-home care options is crucial. This includes services like In Home Hospice Care. These services offer comprehensive support for patients and families, ensuring a higher quality of life throughout recovery. You can also explore related articles by exploring our sitemap.
Beyond Bandages: Wounds That Thrive With Home Care
Not all wounds require the same level of care. Knowing which wounds respond well to in-home treatment is key for effective healing. This guide explores various chronic wound types and how regular home monitoring can significantly improve recovery.
Chronic Wounds: A Case for Consistent Care
Chronic wounds, such as diabetic foot ulcers and venous leg ulcers, often need ongoing care. In-home wound care provides regular monitoring and personalized treatment, both essential for managing these conditions. For instance, diabetic foot ulcers, affecting 15-25% of individuals with diabetes, greatly benefit from the consistent care provided at home. This consistent care, combined with individualized treatment plans, can lead to better healing and fewer complications. Specialized cleaning techniques and advanced dressings, tailored to each patient's needs, further support the healing process.
Post-Surgical and Other Wound Types
Beyond chronic wounds, post-surgical incisions also heal well with professional in-home care. The home environment allows for personalized care that adapts as the wound heals. This adaptability ensures the care plan always meets the patient's current needs. Home care can be vital for managing wounds and supporting overall recovery, particularly when addressing inflammation with methods like those discussed in CBD to Heal Inflammation Across Body. Additionally, burns, pressure injuries, and traumatic wounds can be effectively managed outside of a hospital. In-home wound care offers a comfortable and convenient setting for patients recovering from these various injuries.
Specific Protocols for Home Care Success
Successful in-home wound care relies on specific protocols tailored to each wound type. These protocols include a range of specialized techniques, from advanced dressings to meticulous cleaning methods.
-
Specialized Cleaning: In-home wound care professionals use specialized cleaning techniques to prevent infection and encourage healing. This might involve using specific solutions and gentle debridement.
-
Advanced Dressings: Advanced wound dressings are selected based on the unique needs of each wound. Some dressings keep the wound moist, while others help with drainage.
-
Individualized Care Plans: Each patient receives a personalized care plan addressing their individual needs and situation. This includes a tailored schedule for dressing changes and wound assessments.
To further clarify the various approaches, let's look at the following table:
Common Wound Types and Their In-Home Treatment Approaches
This table categorizes different wound types commonly treated at home and outlines the specific treatment methods, monitoring requirements, and expected healing timeframes for each.
| Wound Type | Treatment Approach | Monitoring Frequency | Average Healing Time |
|---|---|---|---|
| Diabetic Foot Ulcers | Offloading, debridement, specialized dressings, infection control | Daily to weekly, depending on severity | Weeks to months |
| Venous Leg Ulcers | Compression therapy, leg elevation, wound dressings | Weekly to bi-weekly | Several weeks to months |
| Pressure Injuries (Stage I-II) | Pressure relief, regular repositioning, protective dressings | Daily | Several weeks |
| Surgical Incisions | Sterile dressing changes, wound monitoring, pain management | Daily initially, then decreasing frequency | 1-3 weeks depending on the surgery |
| Minor Burns (First-degree) | Cool compresses, pain relief, topical ointments | Daily | A few days to a week |
This table provides a general overview. Individual healing times and treatment approaches will vary based on the specific wound and the patient's overall health.
Recognizing When to Return to Clinical Settings
While in-home wound care offers many advantages, certain signs indicate a need to return to a clinical setting.
-
Increased Pain: Sudden or worsening pain could suggest an infection or other complication.
-
Changes in Wound Appearance: Changes in color, odor, or drainage might signal a problem.
-
Signs of Infection: Fever, chills, redness, or swelling around the wound require immediate medical attention.
In-home wound care professionals are trained to spot these warning signs and will contact the patient's physician to ensure they receive appropriate care. This proactive approach minimizes complications and promotes optimal healing. Understanding these protocols and warning signs helps patients and their families feel confident choosing in-home wound care.
The Tech Revolution in Your Living Room

In-home wound care has evolved beyond simple bandages and antiseptic. Technology now brings professional-level care directly to patients, offering faster healing, lower infection risk, and greater comfort.
Smart Dressings and Portable Devices
Imagine a dressing that communicates with your doctor. Smart dressings use embedded sensors to track temperature, pH, and moisture levels, sending real-time data to healthcare providers. This allows for proactive adjustments to treatment and early detection of complications.
Portable negative pressure wound therapy (NPWT) devices, once confined to hospitals, are now available in portable sizes. These devices offer the same advantages as traditional NPWT, promoting improved blood flow and faster healing.
Telehealth: Bridging the Distance in Wound Care
Telehealth is changing how in-home wound care is delivered. Secure platforms allow specialists to remotely assess wounds using high-resolution images and video consultations. This is especially helpful for patients in rural areas with limited access to specialized clinics.
For example, a specialist can guide a home health nurse through a complex dressing change via video conference, ensuring proper execution. This remote access ensures patients receive appropriate care regardless of location.
Balancing Tradition with Innovation
While technology advances, traditional wound management remains vital. Basic wound care fundamentals, like proper cleaning and dressing application, are still crucial for effective treatment.
Cost and access are also important factors. While advanced technologies are gaining popularity, traditional methods are essential, particularly in areas with limited access to modern treatments. The global market for traditional wound management was valued at approximately USD 5,306.5 million in 2024. It's projected to reach USD 7,014.0 million by 2035, growing at a CAGR of 2.6% between 2025 and 2035. More detailed statistics are available here. Often, combining traditional methods with new technologies offers the most effective and accessible in-home wound care.
Navigating the System: Getting the Care You Deserve
Accessing in-home wound care shouldn't be a maze. This section provides a straightforward guide to getting the care you need, whether you're recovering from surgery or managing a chronic condition.
Understanding Insurance Coverage
Getting your in-home wound care covered by insurance often depends on proper documentation. Your doctor plays a vital role in this. They need to clearly document the medical necessity of in-home care, detailing the wound type, its severity, and the treatment required. Using precise medical terminology strengthens your case.
For example, documenting "a stage III pressure ulcer requiring debridement and specialized dressings" is much more effective than simply writing "a wound on the back." Accurate documentation helps ensure your needs are clearly understood by the insurance provider.
Navigating Medicare, Medicaid, and Private Insurance
Each insurance provider has its own specific requirements for in-home wound care services. Understanding these nuances is key to securing coverage.
-
Medicare Part B: Typically covers in-home wound care if a physician deems it medically necessary. The care must be provided by a Medicare-certified agency.
-
Medicaid: Coverage varies by state, but often includes in-home wound care for those who qualify. Checking with your state's Medicaid office is essential.
-
Private Insurance: Policies can differ significantly. Carefully review your plan details to understand coverage limits and any pre-authorization requirements.
Successfully navigating these systems involves understanding your policy and advocating for what you need. For a more detailed guide, check out our resource on navigating in-home wound care.
Evaluating Potential Providers
Choosing the right in-home wound care provider is critical for effective healing. Consider these key factors:
-
Credentials: Verify that providers have the required licenses and certifications.
-
Experience: Look for providers with a strong track record in treating your specific type of wound.
-
Reputation: Ask your doctor or other healthcare professionals for recommendations.
-
Communication: Choose a provider who communicates clearly and thoroughly addresses all your questions and concerns.
Be mindful of potential red flags, such as providers pushing unnecessary services or lacking proper credentials. A thorough evaluation helps ensure you receive high-quality care.
Exploring Alternative Funding Sources
If you face coverage limitations, explore alternative funding options.
-
Patient Assistance Programs: Many pharmaceutical companies and non-profit organizations offer financial help for specific treatments, including wound care supplies.
-
Community Resources: Your local health department or social service agencies may have programs to help cover in-home care costs.
-
Negotiating Payment Plans: Discuss payment options with your chosen provider. Some may offer flexible plans to make care more affordable.
Exploring these options empowers you to receive necessary care, regardless of financial constraints. In-home wound care is valuable and can dramatically improve healing and quality of life. By understanding the system and advocating for yourself, you can access the care you deserve. Taking a proactive approach can greatly improve your healing journey and overall well-being. Remember, healing at home is about more than just convenience; it’s about getting the best possible results in a comfortable and familiar setting.
Becoming Your Own Wound Care Advocate
The most successful in-home wound care happens when patients and their caregivers actively participate in the healing process. This involves understanding the wound care process and working closely with healthcare professionals. It's truly about empowering individuals and their families to take charge of their well-being.
Empowering Patients Through Knowledge
Wound care educators play a vital role in equipping families with the knowledge and skills they need. They offer hands-on training in practical techniques, like wound cleaning and dressing changes. This empowers caregivers to confidently manage these tasks at home between visits from healthcare professionals.
For example, understanding how to properly clean a wound minimizes the risk of infection. Knowing the correct way to change dressings helps promote faster healing. These skills are essential for supporting the healing process at home.
Setting Up a Home Wound Care Station
Creating a dedicated wound care station at home simplifies the entire caregiving process. This means gathering all the necessary supplies and organizing them in a logical and efficient manner. Think of it as your own personal mini-clinic conveniently located in your home.
-
Essential Supplies: Be sure to stock up on essential items like sterile gloves, gauze, bandages, antiseptic wipes, and any prescribed ointments. Keeping everything together in one location saves valuable time and reduces stress.
-
Organization Tips: Use clear containers to store supplies and label everything clearly. This makes it easy to find what you need quickly during dressing changes. A rolling cart can be a great addition, keeping all your supplies mobile and readily accessible.
Managing Common Challenges
In-home wound care can present challenges, but being aware of these beforehand helps you find solutions.
-
Dressing Adhesive Sensitivities: Some people have sensitive skin and can experience irritation from adhesive dressings. Using hypoallergenic options or skin barrier wipes can help alleviate discomfort.
-
Pain Management: Pain is common during dressing changes. Consider pain relief methods like applying a numbing cream before changing the dressing or using over-the-counter pain relievers to make the experience more bearable.
Communication: The Key to Successful Collaboration
Open communication between home caregivers and professional healthcare providers is paramount. Regular check-ins and clear communication about any changes in the wound are crucial. For instance, if a caregiver notices increased redness, swelling, or drainage, they should contact their healthcare provider immediately.
Active participation in discussions about the treatment plan is essential. This gives patients a sense of control and fosters a collaborative approach to care. By understanding these factors, individuals and their families can become effective advocates for their own well-being. This approach not only leads to better outcomes but also empowers patients to play an active role in their recovery.

