The Hidden Crisis: Understanding Pressure Ulcer Impact

Pressure ulcers, also known as bedsores or pressure sores, pose a significant challenge in healthcare. These wounds develop due to prolonged pressure on the skin, restricting blood flow to the affected area. This can affect anyone who remains immobile for extended periods, particularly individuals with limited mobility. Understanding the impact of these ulcers goes beyond the immediate physical discomfort.
The True Cost of Pressure Ulcers
Pressure ulcers have widespread consequences, affecting both the patient and the healthcare system. For individuals, pressure ulcers cause significant pain, limit mobility, and can lead to serious infections.
These complications often necessitate extended hospital stays and complex wound care, significantly impacting quality of life. The financial burden associated with treatment is also substantial. Increased healthcare costs are a direct result of the prolonged care, specialized treatments, and resources required to manage these wounds.
Pressure ulcers represent a significant global health issue, with a prevalence rate of approximately 12.8% worldwide. This is particularly problematic in healthcare settings, leading to extended hospital stays and increased costs. Historically, management involved regular patient repositioning to redistribute pressure.
More recently, comprehensive care bundles, such as the NHS 'aSSKINg' model, have been introduced. This model focuses on risk assessment, skin health, nutrition, and mobility. Despite these advancements, pressure ulcers remain a persistent challenge, particularly among aging populations and those with chronic conditions, where incidence continues to rise. Learn more about pressure ulcer prevalence and historical management.
Beyond Pressure: Other Contributing Factors
While sustained pressure is the primary cause, other factors contribute to pressure ulcer development. Friction, the force of skin rubbing against a surface like bedding, weakens the skin and increases vulnerability.
Shear occurs when skin and underlying bone move in opposite directions, such as when sliding down in bed or a chair. This damages underlying blood vessels, leading to tissue breakdown. The skin's microclimate, including temperature and moisture levels, also plays a crucial role.
Excessive moisture from perspiration or incontinence softens the skin, increasing the risk of breakdown. Conversely, excessively dry skin can crack and become prone to injury.
Why Prevention Is Paramount
Considering the complexity of pressure ulcers and their impact, prevention is essential. Effective prevention strategies minimize patient suffering and reduce the burden on healthcare resources.
By understanding how to prevent these ulcers, we can improve patient outcomes and create a more sustainable healthcare system. This involves addressing the root causes and implementing proactive strategies to mitigate their effects. The following sections will explore these strategies, providing practical guidance on prevention in various care settings.
Identifying Vulnerability: Who's Really at Risk?
Identifying those at risk for pressure ulcers is vital for proactive prevention. While immobility is a major factor, the risk extends beyond this. It includes various factors often missed until skin breakdown happens. Understanding these factors helps caregivers and healthcare professionals take preventative action before visible damage.
Recognizing the Subtle Signs
Recognizing subtle warnings is crucial for early intervention. These can include changes in skin color, like redness or discoloration that doesn’t fade quickly. Also, skin that feels warmer or cooler than surrounding areas can signal compromised circulation.
Changes in skin texture, such as increased firmness or softness, should also be noted. These subtle shifts often come before visible skin breakdown and require immediate attention. Early detection and intervention can prevent progression to more serious pressure ulcer stages.
Medical Conditions and Increased Vulnerability
Some medical conditions significantly raise the risk of pressure ulcers, even when patients seem stable. Conditions impacting circulation, like diabetes and peripheral artery disease, reduce blood flow to the skin, increasing susceptibility to damage.
Neurological conditions affecting sensation, like spinal cord injuries, can prevent individuals from feeling pain or discomfort, hindering early detection of pressure-related problems. Conditions weakening the immune system, like cancer or HIV/AIDS, impair healing, raising the risk of infection in existing pressure ulcers. Understanding overall well-being is crucial; for more on overall wellness, explore resources on workplace mental health.
Assessing and Documenting Risk
Professional tools like the Braden Scale help assess pressure ulcer risk in clinical settings. This scale evaluates sensory perception, moisture, activity, mobility, nutrition, and friction/shear. Each factor receives a score, and a lower total score indicates higher risk.
For home caregivers, simplified approaches focusing on these same principles can be effective. Regularly checking for changes in skin color, temperature, and texture over bony areas is essential.
Understanding the statistical context of pressure ulcers is also important. A systematic review indicated a global incidence of about 12%. However, prevalence can vary from 8.3% to 23% in European hospitals and between 8% and 40% in the United States. Common locations include the sacrum, buttocks, heels, and trochanters. More detailed statistics can be found here.

The following table outlines key risk factors for pressure ulcers, along with their relative impact and prevention methods.
Common Pressure Ulcer Risk Factors
| Risk Factor | Level of Risk | Prevention Strategies |
|---|---|---|
| Immobility | High | Frequent repositioning, pressure-relieving surfaces |
| Impaired Circulation | High | Optimize blood flow, manage underlying conditions |
| Impaired Sensation | High | Regular skin checks, pressure redistribution |
| Moisture | Moderate | Keep skin clean and dry, use barrier creams |
| Friction/Shear | Moderate | Minimize friction and shear forces during movement |
| Poor Nutrition | Moderate | Ensure adequate protein and calorie intake |
This table summarizes the main risk factors for pressure ulcer development and emphasizes the importance of proactive prevention strategies.
Practical Techniques for Documentation
Consistently documenting risk factors ensures consistent care across different caregivers and settings. A simple chart noting observations, interventions, and skin changes provides valuable data. This information helps track progress, identify trends, and ensure everyone involved in the patient's care is informed and working towards the same preventative goals. This careful documentation is especially important for those with multiple caregivers or those transitioning between care settings.
The Movement Revolution: Positioning That Protects

Moving away from traditional, fixed turning schedules is essential for preventing pressure ulcers. This involves a more dynamic, science-based method of positioning and movement. Proper repositioning significantly improves pressure distribution, benefiting a patient's comfort and overall health. This section explores how smart repositioning techniques can drastically lower the risk of pressure ulcers.
The Science of Smart Repositioning
Regular repositioning relieves pressure on vulnerable areas, improving blood flow to the skin and underlying tissues. But it's not just about how often; the method of repositioning matters just as much. The 30-degree tilt, for instance, is a proven technique that greatly reduces pressure on bony areas like the sacrum and heels without affecting sleep or comfort.
Pillows and wedges can further improve pressure distribution and support proper body alignment. This creates a more comfortable and safer environment for patients.
Addressing Psychological Barriers
Starting a movement program isn't always simple. Patients may resist repositioning due to pain, discomfort, or simply wanting uninterrupted rest. Motivational strategies are crucial here. Clearly explaining how repositioning reduces pain and speeds up healing can encourage patient cooperation.
Involving patients in their care plan, letting them choose preferred positions and repositioning times when possible, empowers them and increases compliance. This patient-centered approach fosters a sense of control and leads to better outcomes.
The Global Burden of Pressure Ulcers
The global impact of pressure ulcers has seen a worrying increase. Between 1990 and 2021, the number of cases worldwide jumped from 300,442 to 645,588. While the overall prevalence rate has dipped slightly, deaths from pressure ulcers rose from 16,622 to 37,033 during the same period. This underscores the continued need for effective prevention strategies. Find more detailed statistics here.
Practical Guidance for Caregivers
Caregivers, particularly those with limited strength, might find frequent repositioning difficult. Practical guidance and assistive devices are invaluable in these situations. Using slide sheets or transfer boards can reduce strain, making repositioning easier and safer for both the caregiver and patient.
Small, frequent movements throughout the day, like shifting weight or adjusting limb positions, can also significantly reduce pressure buildup. This proactive approach minimizes the need for major repositioning.
Innovative Approaches for Maintaining Schedules
Keeping up with repositioning schedules can be tough with limited staff, a common problem in many healthcare settings. This calls for innovative solutions. A team approach, where several caregivers share the responsibility of repositioning patients, can effectively distribute the workload.
Technology, such as reminder apps or pressure mapping systems, can also improve adherence to schedules and provide valuable data for improving repositioning strategies. This integration of technology enhances the efficiency and effectiveness of pressure ulcer prevention.
Skin Care Strategies That Actually Prevent Breakdown
Effective skin care plays a vital role in preventing pressure ulcers. It's more than just basic hygiene; it's about actively protecting and strengthening the skin's natural barrier. This approach minimizes the risk of breakdown and promotes faster healing if damage does occur. This involves understanding moisture management, recognizing early warning signs, and choosing the right products.
Maintaining the Delicate Balance: Moisture Management
Managing skin moisture is a balancing act. Too much moisture, like from incontinence or sweating, softens the skin and makes it vulnerable to friction and shear. But overly dry skin can crack and become just as susceptible to injury.
The goal is to keep skin clean and dry without removing its natural oils. Use gentle cleansers and moisturizers designed for sensitive skin. Avoid harsh soaps and hot water, as these can damage the skin's protective barrier. For those dealing with incontinence, frequent changes and the use of barrier creams or ointments can help prevent moisture-associated skin damage (MASD).
Recognizing the Early Warning Signs
Spotting early signs of skin breakdown allows for quick action before ulcers develop. Watch for redness that doesn't disappear after pressure is removed, changes in skin temperature (either hotter or colder than surrounding skin), and texture changes like increased firmness or a boggy feel.
Blistering or skin discoloration can also signal impending breakdown. These changes often appear over bony areas like the heels, sacrum, elbows, and hips. Any of these signs should prompt immediate action, including repositioning, pressure relief, and a thorough skin assessment.
Choosing the Right Products for Prevention
Choosing the right skin care products is essential. Look for pH-balanced cleansers free of fragrances and harsh chemicals. Moisturizers should be formulated for dry or sensitive skin and absorb easily without leaving a greasy residue.
Barrier creams and ointments protect against moisture while allowing the skin to breathe. For individuals with existing skin damage, specialized products that promote healing might be needed. Consulting with a wound care specialist, such as those at Rapid Wound Care, can help ensure you select the most effective products. They can offer expert guidance and personalized treatment plans.
Practical Protocols for Different Skin Types
Different skin types require tailored approaches. Fragile elderly skin benefits from gentle handling and regular moisturizing to combat dryness and thinning. For individuals with moisture-associated dermatitis, meticulous hygiene and breathable barrier products are essential.
Creating a personalized skin care plan based on individual needs is crucial. This could involve adjusting how often you cleanse and moisturize, using specific products for different areas, and carefully monitoring for any changes in skin condition. This proactive, personalized approach optimizes pressure ulcer prevention and improves overall skin health.
Surface Solutions: Choosing Equipment That Delivers Results
The data chart below visualizes performance metrics and pressure distribution characteristics across different support surfaces.
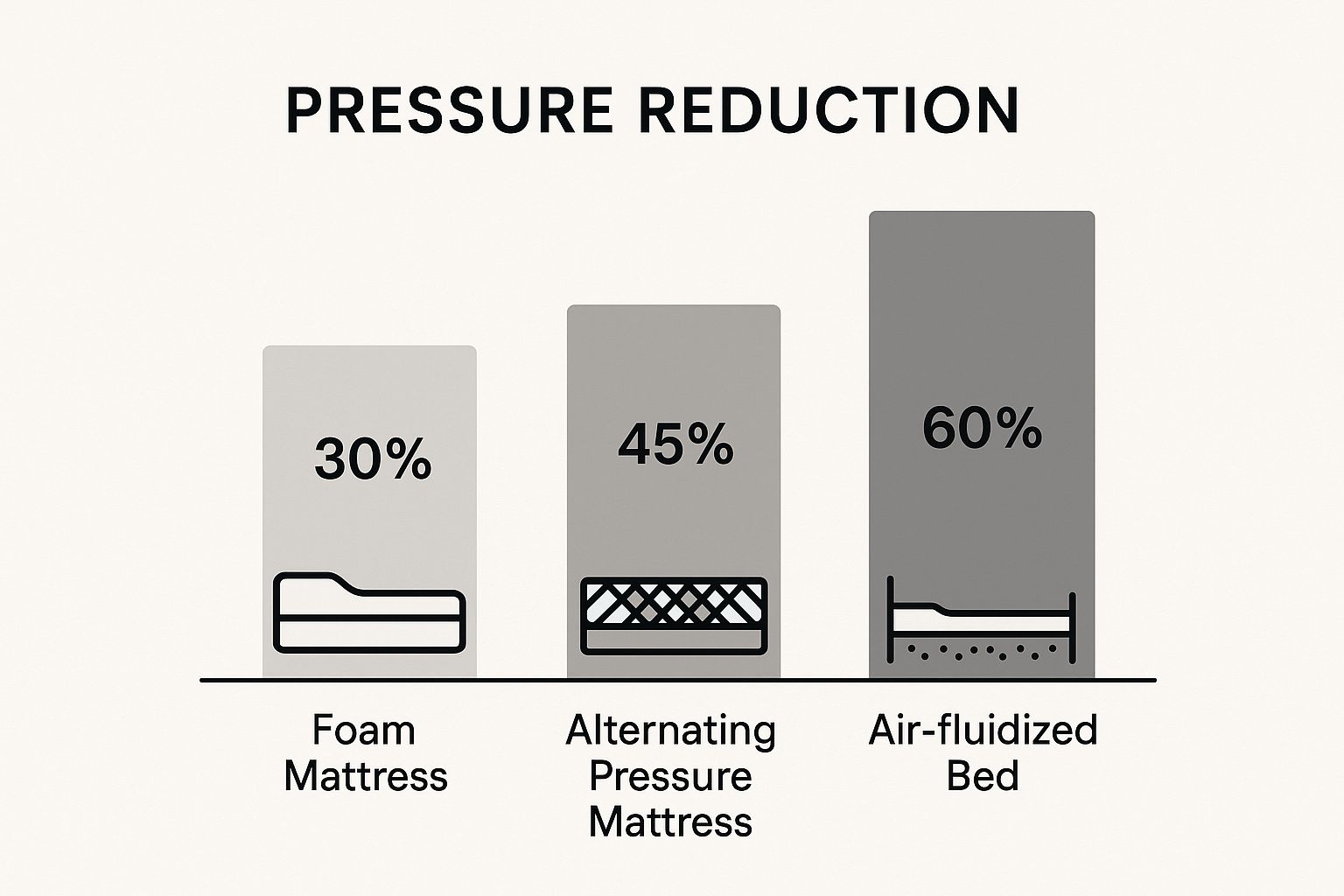
This data chart highlights how each surface redistributes pressure and protects vulnerable skin, showing that more advanced models shift load more effectively than basic options.
Choosing the right support surface is crucial for preventing pressure ulcers. It's not just about comfort; it's about effective pressure redistribution and safeguarding sensitive areas. To select equipment that performs in real-world conditions, we need to look past marketing and focus on actual results.
Understanding Support Surface Options
Support surfaces vary from foam mattresses to alternating pressure mattresses. Key categories include:
- Foam Mattresses: Basic pressure redistribution for low-risk patients
- Static Air Mattresses: Even air distribution, ideal for moderate-risk cases
- Alternating Pressure Mattresses: Dynamic inflation cycles to shift pressure
- Low-Air-Loss Beds: Continuous airflow to manage moisture and reduce shear
Each option targets different risk levels, so understanding their mechanisms is the first step in matching surface to patient needs.
Matching Surface To Risk Level
A patient's risk assessment guides surface selection:
- Low Risk: Foam overlays or standard cushions
- Moderate Risk: Static air or gel-infused surfaces
- High Risk: Alternating pressure mattresses or low-air-loss beds
Correct pairing ensures adequate pressure redistribution and supports blood flow to vulnerable areas.
Evaluating Equipment Effectiveness
Regular checks keep support surfaces performing correctly:
- Inspect skin for redness or early breakdown
- Monitor for persistent pressure points or discomfort
- Adjust mattress settings or replace the surface if issues persist
When standard checks aren’t enough, consult a specialist to explore alternative surfaces or fine-tune settings.
Cost Versus Benefit: Making Informed Decisions
Costs for support surfaces can range significantly:
- Foam Mattresses: $100–300
- Static Air Mattresses: $100–300
- Alternating Pressure Mattresses: $500–1500
- Low-Air-Loss Beds: $1500–3000
A bar chart (see infographic) outlines these ranges, showing how price increases with complexity and advanced features. Weighing cost against patient risk and insurance coverage helps ensure the best match without unnecessary expense.
To help you compare options, the table below outlines key characteristics, benefits, and cost ranges.
Comparison of Pressure-Reducing Support Surfaces
This table compares different types of support surfaces used in pressure ulcer prevention, including their mechanisms, benefits, limitations, and ideal applications
| Support Surface Type | Mechanism of Action | Best For | Limitations | Approximate Cost Range |
|---|---|---|---|---|
| Foam Mattress | Pressure redistribution through viscoelastic foam | Low-risk patients | Limited long-term support | $100–300 |
| Static Air Mattress | Even air distribution across sealed chambers | Moderate-risk individuals | Requires regular inflation checks, heat buildup | $100–300 |
| Alternating Pressure Mattress | Cycles inflation and deflation to shift pressure points | High-risk patients | Periodic repositioning needed, can be noisy | $500–1500 |
| Low-Air-Loss Bed | Continuous airflow manages microclimate and pressure | High-risk with moisture concerns | High purchase and maintenance cost | $1500–3000 |
From this comparison, you can see that as surfaces become more advanced, costs rise but so do pressure-relief features. Choosing the right surface means balancing patient risk with budget and support requirements.
Practical Assessment Techniques
Simple in-bed tests confirm adequate pressure relief:
- Place a hand under the surface to feel for pressure points
- Observe how quickly the material rebounds after weight shifts
- Spot-check bony prominences to ensure even support
If you notice areas that stay compressed or the surface fails to recover shape, consider upgrading or adjusting the equipment. For specialized guidance on assessing and selecting the right surface, consult the professionals at Rapid Wound Care. They provide personalized evaluations and clear recommendations.
Nutrition's Critical Role in Skin Defense
Proper nutrition is fundamental to preventing pressure ulcers. Think of your skin as a fortress, and nutrients are the essential building blocks that maintain its strength and resilience. This section explores how specific nutrients bolster skin health and addresses nutritional challenges in various care settings.
The Building Blocks of Healthy Skin: Key Nutrients
Certain nutrients are especially crucial for maintaining skin integrity and promoting healing. Protein, for instance, is essential for cell regeneration and the production of collagen, the protein that gives skin its structure and strength. Without adequate protein, skin becomes thin and fragile, increasing the risk of breakdown.
Vitamins A and C also play vital roles. Vitamin A supports cell growth and repair, while Vitamin C is crucial for collagen synthesis and wound healing. These vitamins work in concert to fortify the skin's defenses against pressure and friction. Proper nutrition is a cornerstone of healthy skin; learn more about senior meal prep.
Ensuring Adequate Protein Intake
For individuals at risk of pressure ulcers, sufficient protein intake is non-negotiable. It helps repair damaged tissues and maintain the skin's protective barrier. This can be challenging, especially for those with a poor appetite or swallowing difficulties.
Strategies for increasing protein intake include adding protein powder to beverages, incorporating high-protein snacks like nuts and yogurt, and choosing protein-rich meals featuring lean meats, fish, eggs, and beans. These simple adjustments can make a significant difference in skin health and overall well-being.
Addressing Nutritional Challenges
Real-world barriers to optimal nutrition exist, including decreased appetite, swallowing difficulties, and limited food budgets. These challenges are particularly common in long-term care settings and among individuals with chronic illnesses.
Creative solutions are necessary to overcome these obstacles. Offering smaller, more frequent meals can be more appealing than large portions, for example. Pureed or softened foods can help those with chewing or swallowing difficulties maintain adequate nutrition. Collaborating with a registered dietitian can help tailor meal plans to individual needs and preferences within budgetary constraints.
Navigating the World of Supplements
The supplement market offers a plethora of products claiming to boost skin health. However, not all supplements are created equal. Some, like vitamin C and zinc, have demonstrated promise in supporting wound healing and collagen production.
Others lack sufficient scientific evidence to support their claims. It's essential to consult with a healthcare professional before beginning any new supplement regimen, especially for individuals with underlying medical conditions. They can determine which supplements are appropriate and safe for individual needs.
Practical Tips for Improving Nutrition
Here are some actionable strategies for improving nutrition in individuals at risk of pressure ulcers:
-
Focus on whole foods: Prioritize fruits, vegetables, whole grains, and lean protein sources.
-
Hydration is key: Encourage regular fluid intake to maintain skin hydration.
-
Meal planning: Create balanced meals that incorporate essential nutrients.
-
Monitor weight: Track weight regularly to identify potential nutritional deficiencies.
By implementing these strategies, we can strengthen skin from the inside out, providing a vital layer of defense against pressure ulcers. For expert guidance on wound care and personalized treatment plans, including nutritional support, consult the professionals at Rapid Wound Care.
Specialized Prevention For Unique Patient Populations
Preventing pressure ulcers requires a nuanced approach, understanding that one-size-fits-all strategies aren't always effective. Vulnerable populations, like those with spinal cord injuries, end-stage diseases, or specific medical conditions, need tailored preventative measures. This section explores adapting pressure ulcer prevention for these distinct groups and across various care settings.
Tailoring Prevention For Spinal Cord Injuries
Individuals with spinal cord injuries (SCI) have a significantly higher risk of pressure ulcers due to reduced sensation and mobility. Regular repositioning is vital and often requires specialized equipment and techniques. Pressure-relieving cushions and mattresses designed for SCI patients help distribute weight and minimize pressure on bony areas. Skin checks are essential, focusing on areas susceptible to pressure, such as the sacrum, heels, and ischial tuberosities.
Maintaining skin integrity is also paramount. Keeping skin clean and dry is crucial, particularly for those with incontinence. Proper nutrition plays a critical role in preventing pressure ulcers in SCI patients. Adequate protein and calorie intake supports tissue repair and overall health.
Addressing End-Stage Disease Considerations
Patients with end-stage diseases face unique challenges in pressure ulcer prevention. Their compromised immune systems, combined with decreased mobility and altered nutritional status, increase vulnerability. Pressure ulcer prevention in this group emphasizes comfort and dignity. Frequent skin assessments, gentle repositioning, and pressure-relieving surfaces are essential.
Pain management is another crucial aspect. Pressure ulcers can cause significant pain, impacting quality of life. Working with a palliative care team can address pain and ensure the patient's comfort.
Adapting Prevention Across Care Settings
Prevention strategies must adapt to different care settings, from acute care hospitals to long-term care and home environments. In acute care, early assessment, frequent repositioning, and meticulous skin care are key. Long-term care requires ongoing monitoring, individualized care plans, and staff education for consistent prevention.
Home environments present distinct challenges due to limited resources and caregiver support. Teaching family members and caregivers about repositioning, skin care, and nutrition is essential. Adapting prevention at home means creating a sustainable care plan considering available resources and caregiver capabilities.
Coordinating Care Among Interdisciplinary Teams
Effective pressure ulcer prevention relies on coordinated efforts among healthcare professionals, including nurses, physicians, therapists, and dietitians. Clear communication, shared goals, and consistent prevention strategies are critical. Interdisciplinary team meetings can facilitate communication and ensure everyone is aligned.
Regular documentation and updates on skin condition and overall risk are vital for care coordination. This collaborative approach ensures a comprehensive strategy to minimize pressure ulcer risk.
Addressing Resource Constraints
Resource limitations, especially staffing shortages, can hinder prevention. Creative solutions are needed. Appropriately delegating tasks, using technology like reminder apps, and implementing streamlined protocols can optimize resource allocation.
Involving family members and caregivers can also lessen the burden on healthcare professionals. This collaborative approach helps ensure consistent patient care, even with limited resources.
For comprehensive wound care, including specialized prevention and personalized treatment, contact the experts at Rapid Wound Care. Their certified professionals provide at-home care and support for various wound types, including pressure ulcers, ensuring optimal healing and improved well-being.

