Decoding Chronic Wounds: Beyond the Surface
Chronic wounds pose a significant challenge within the healthcare system, requiring specialized chronic wound care. Unlike acute wounds, which heal relatively quickly, chronic wounds persist for extended periods, often exceeding 8 weeks. This delayed healing isn't just a minor setback; it significantly impacts a patient's quality of life and places a considerable burden on healthcare resources. Understanding the intricacies of these wounds is paramount for effective treatment and improved patient outcomes.
Understanding the Complexity of Chronic Wounds
What exactly defines a wound as "chronic"? Essentially, it's a disruption in the normal healing trajectory. Acute wounds progress through predictable stages, while chronic wounds stall, often due to underlying factors hindering tissue repair. These factors can include inadequate blood circulation, persistent infection, uncontrolled inflammation, and cellular dysfunction. This means traditional wound care, effective for acute injuries, often proves insufficient for addressing the root causes of chronic wounds.
For instance, a minor scrape typically heals within a couple of weeks. However, a diabetic foot ulcer can persist for months or even years. This stark contrast underscores the necessity for specialized chronic wound care that delves deeper than simply covering the wound. Effective treatment demands a comprehensive approach, considering the individual's overall health, the specific wound type, and the underlying causes contributing to its chronicity.
The infographic below visually represents the prevalence, average healing time, and recurrence rate of common chronic wounds.
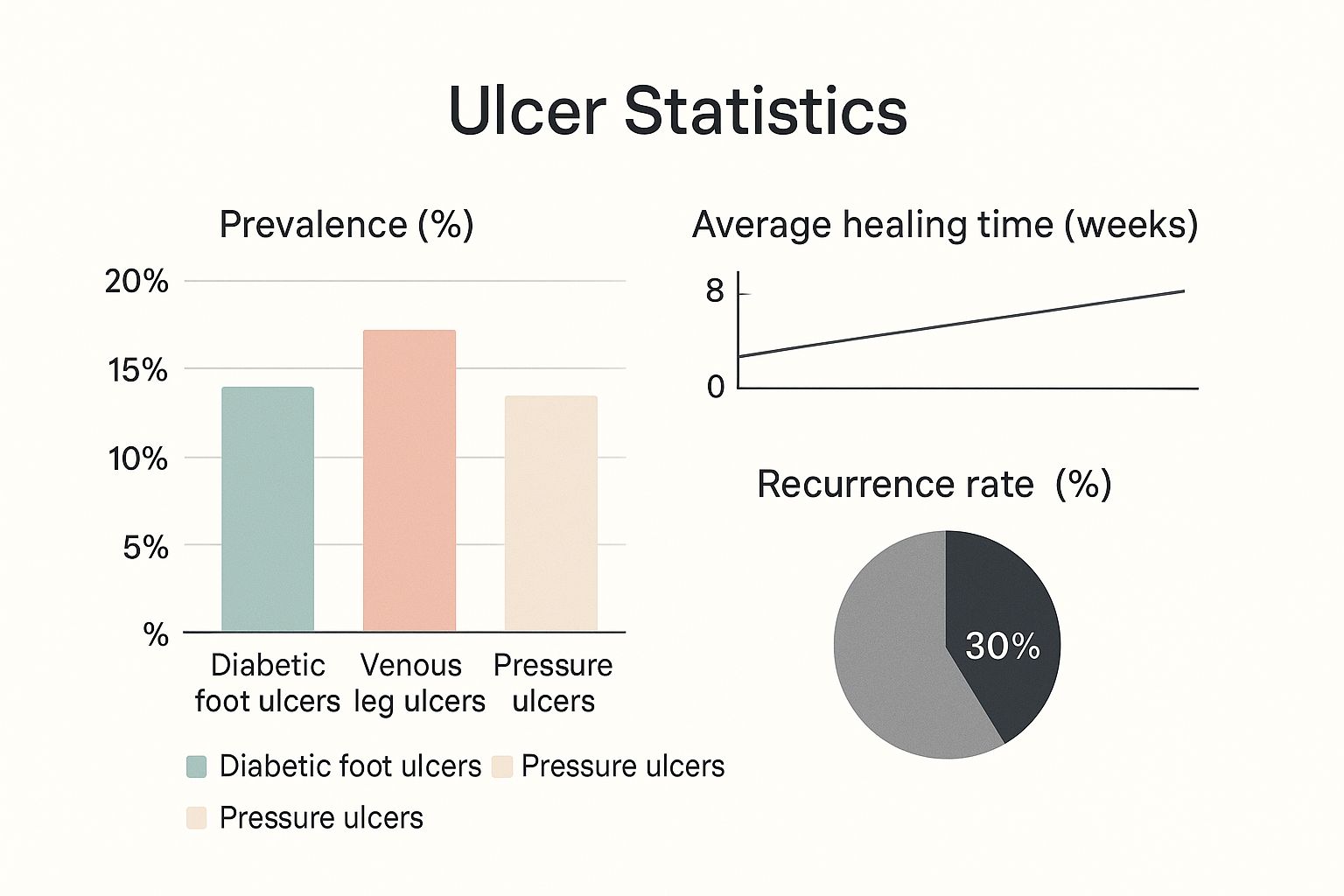
As shown, venous leg ulcers are the most prevalent, followed by diabetic foot ulcers and pressure ulcers. The significant recurrence rate of 30% emphasizes the importance of continuous chronic wound care and preventative strategies. This further reinforces the need for comprehensive care that addresses not just the immediate wound but also the underlying conditions and patient-specific factors.
Common Types of Chronic Wounds
Different chronic wounds present unique challenges. Diabetic foot ulcers, often arising from nerve damage and reduced blood flow, require careful glucose management and pressure offloading. Pressure injuries, typically forming over bony prominences, necessitate frequent repositioning and specialized support surfaces. Venous ulcers, commonly found in the lower legs, benefit from compression therapy to enhance circulation. Arterial wounds, caused by poor arterial blood flow, might require procedures to restore adequate circulation.
To better understand the various types of chronic wounds, their causes, and characteristics, consult the table below:
Common Types of Chronic Wounds: A comparison of different chronic wound types, their prevalence, and distinctive characteristics
| Wound Type | Prevalence (%) | Primary Causes | Typical Location | Distinguishing Features |
|---|---|---|---|---|
| Venous Leg Ulcers | 40-60 (Estimated based on infographic) | Venous insufficiency, valve dysfunction | Lower legs, ankles | Shallow, irregular shape, often with heavy drainage |
| Diabetic Foot Ulcers | 15-25 (Estimated based on infographic) | Nerve damage (neuropathy), poor circulation | Feet, toes | Deep, often painless initially, can lead to infection and amputation |
| Pressure Ulcers | Varies widely | Prolonged pressure on skin, friction, shear | Bony prominences (e.g., heels, sacrum, hips) | Staged based on depth of tissue damage |
| Arterial Ulcers | ~10 (Estimated based on lower prevalence compared to others) | Peripheral artery disease (PAD), reduced blood flow | Toes, feet, heels | Deep, painful, "punched-out" appearance, dry and pale wound bed |
This table provides a quick overview of common chronic wound types, their contributing factors, and key features that aid in identification and management. Accurate diagnosis and tailored treatment plans are essential for effective chronic wound care.
The Growing Chronic Wound Care Market
The global market for chronic wound care is expanding significantly. Valued at approximately $15.27 billion in 2024, it's projected to reach around $16.47 billion by 2025, demonstrating a compound annual growth rate (CAGR) of about 7.8%. This growth is primarily fueled by the rising prevalence of diabetes, obesity, and an aging global population, all contributing to increased chronic wound incidence. More detailed statistics can be found here.
Security in Chronic Wound Care
Effective chronic wound care programs also require addressing security concerns for healthcare professionals. Security awareness training for healthcare is a valuable resource, particularly given the increasing threat of data breaches and cybersecurity incidents in today's healthcare landscape.
Assessment Strategies That Actually Reveal Healing Barriers
Effective chronic wound care depends on accurate assessment. Instead of simply measuring a wound's length and width, a comprehensive approach considers various factors affecting healing. This involves combining systematic evaluation tools and clinical judgment to understand the wound's status and the patient's overall health.
Key Components of Comprehensive Wound Assessment
Accurate wound assessment goes beyond basic measurements. It involves examining the wound's specifics and the patient's condition. This includes analyzing wound tissue, assessing the surrounding skin, and evaluating the patient's overall health.
-
Wound Measurement: Precisely measuring the wound's size (length, width, depth) and area establishes a baseline for tracking progress.
-
Tissue Identification: Identifying the tissue types within the wound bed (e.g., granulation tissue, slough, eschar) provides insights into the healing phase and potential barriers. For example, necrotic tissue signals the need for debridement.
-
Periwound Assessment: Examining the skin around the wound for inflammation, infection, maceration, or dryness reveals clues about the wound's environment and potential complications.
-
Patient Factors: A thorough assessment considers the patient's overall health, including nutrition, mobility, pain level, and underlying medical conditions that could influence healing. This holistic perspective is crucial for an effective chronic wound care plan.
Advanced Diagnostic Technologies
Emerging diagnostic technologies enhance our ability to assess wounds.
-
Infrared Imaging: This non-invasive technique assesses tissue temperature and blood flow, providing information about the wound's vascularity and healing potential.
-
Ultrasound: Ultrasound visualizes underlying tissue structures and blood vessels, helping identify deep infections or other complications not visible on the surface.
-
Hyperspectral Analysis: This technology analyzes the light reflected from the wound, detailing tissue composition and oxygenation. It can detect early signs of infection or other abnormalities.
These tools offer valuable insights into the wound's status and guide treatment decisions, essential for effective chronic wound care.
The Importance of Clinical Intuition
While technology is increasingly important, clinical experience and intuition remain invaluable. Experienced clinicians recognize subtle signs and patterns that even the most advanced technologies might miss. Integrating objective data with clinical judgment is essential for accurate assessment and personalized treatment.
For example, a clinician might notice a change in the wound's odor or drainage, prompting further investigation even if wound measurements haven't changed significantly. You might be interested in: How to master preventing pressure sores.
Putting It All Together
By combining these assessment strategies, clinicians gain a deeper understanding of the barriers hindering wound healing. This comprehensive approach enables targeted interventions addressing the problem's root causes, not just managing symptoms. This shift improves patient outcomes and quality of life for those with chronic wounds.
The Science of Dressing Selection: Matching Products to Wounds

Choosing the right wound dressing from the many available can be a daunting task. This section simplifies the selection process by focusing on practical advice from wound specialists for effective chronic wound care. We’ll cut through the marketing jargon to get to the core of what works.
The TIME Framework: A Guide to Evidence-Based Selection
The TIME framework provides a helpful approach to dressing selection. TIME stands for Tissue, Infection, Moisture, and Edge. This framework encourages a systematic evaluation of the wound and surrounding tissue.
For instance, a wound with a lot of drainage (moisture) will need a highly absorbent dressing. Conversely, a dry wound needs a dressing that helps retain moisture. Understanding the wound's condition is the first step. Then, using the TIME principles, the appropriate dressing is selected. This ensures the dressing supports healing and addresses the specific needs of the wound. Check out our guide on How to master helping wounds heal faster.
Debridement: Preparing the Wound Bed
Debridement, the removal of dead tissue, is often crucial for effective chronic wound care. There are several methods, each with pros and cons. Sharp debridement, using surgical instruments, quickly removes dead tissue but requires a trained healthcare professional. Autolytic debridement uses the body's enzymes for a gentler, though slower, approach.
Other methods include enzymatic debridement, using topical agents, and mechanical debridement, using irrigation or wet-to-dry dressings. The best choice depends on the wound, the patient's health, and available resources. Choosing the right approach is essential for preparing the wound bed for healing.
Exploring Dressing Categories: From Simple to Advanced
The wide array of wound dressings can be confusing. Understanding their functions helps simplify selection.
- Alginates: Derived from seaweed, these are highly absorbent and ideal for heavily draining wounds.
- Foams: These cushion and insulate, creating a moist environment while absorbing moderate drainage.
- Hydrocolloids: Forming a gel-like barrier, these protect the wound and promote autolytic debridement.
- Hydrogels: These moisture-rich dressings soothe and hydrate dry wounds, aiding tissue regeneration.
- Antimicrobial Dressings: These dressings contain agents like silver or iodine to help control infection.
This list highlights the varied functions of common dressings. Understanding these properties allows clinicians to match dressings to specific wound needs.
Cost-Effectiveness and Patient Comfort: Key Considerations
Cost-effectiveness is important in chronic wound care because treatment is ongoing. While advanced therapies can be beneficial, simpler options are often just as effective. Patient comfort is also vital for treatment adherence. Dressings that minimize pain during changes and allow for comfortable movement encourage patient compliance and improve outcomes.
The global chronic wound care market is significant. Valued at approximately $18.7 billion in 2025, it's projected to reach about $27 billion by 2035, growing at a CAGR of 3.8%. This growth is driven by the rise in conditions like diabetes and obesity. See more detailed statistics here.
To help guide dressing selection, we've created the following table summarizing key characteristics of different dressing types:
Wound Dressing Selection Guide
Comprehensive guide to selecting appropriate dressings based on wound characteristics.
| Dressing Type | Best For | Absorption Level | Change Frequency | Special Considerations | Cost Range |
|---|---|---|---|---|---|
| Alginates | Heavily draining wounds | High | 1-3 days | Not for dry wounds | Moderate |
| Foams | Moderate drainage, cushioning | Moderate | 1-3 days | Can be bulky | Moderate to High |
| Hydrocolloids | Dry to lightly draining wounds, autolytic debridement | Low to Moderate | 3-7 days | Not for infected wounds | Low to Moderate |
| Hydrogels | Dry wounds, promoting hydration | Low | 1-3 days | Can macerate surrounding skin | Moderate |
| Antimicrobial Dressings | Infected wounds | Varies | Varies depending on the antimicrobial agent | Can be expensive | Moderate to High |
This table offers a quick overview of dressing options. Remember, selecting the right dressing requires careful consideration of the individual wound characteristics and patient needs.
By considering tissue, infection, moisture, edge, debridement needs, dressing properties, cost, and patient comfort, clinicians can make the best decisions for effective healing and improve patients' quality of life. This careful approach is central to best practices in chronic wound care.
Breakthrough Therapies Transforming Chronic Wound Outcomes

Chronic wounds pose a significant challenge in healthcare. However, ongoing advancements in therapies offer renewed hope for effective healing. This section explores some of the most promising treatments transforming the field of chronic wound care, moving beyond traditional methods to address these persistent conditions.
Negative Pressure Wound Therapy: Creating an Optimal Healing Environment
Negative pressure wound therapy (NPWT), also known as vacuum-assisted closure, has significantly changed the approach to chronic wound care. This innovative therapy involves applying controlled negative pressure to the wound bed. This promotes fluid removal, reduces swelling (edema), and encourages the formation of healthy granulation tissue. NPWT creates an optimal healing environment by gently drawing wound edges closer and increasing blood flow to the affected area. This can be especially helpful for deep or complex wounds.
However, NPWT isn’t suitable for all wounds. Factors like the presence of exposed blood vessels, untreated bone infections (osteomyelitis), or cancerous tissue within the wound need careful consideration before starting this therapy. Appropriate patient selection and meticulous application are also crucial for the best results.
Bioengineered Tissues and Skin Substitutes: Supporting Tissue Regeneration
Bioengineered tissues and skin substitutes offer another advanced approach to chronic wound care. These innovative products act as temporary coverings, protecting the wound and facilitating tissue regeneration. They provide a framework or scaffold for new cells to grow on, thereby speeding up the healing process. Some skin substitutes even contain growth factors that further enhance tissue repair.
These advanced therapies are particularly beneficial for wounds that haven't responded to conventional treatments. For instance, they’ve shown significant success in treating diabetic foot ulcers and venous leg ulcers. However, factors like cost and the need for specialized training for healthcare professionals can limit their wider use.
Cellular Therapies and Growth Factors: Promoting Natural Healing
Cellular therapies and growth factors represent a promising area in chronic wound care, harnessing the body’s own healing potential. Growth factors stimulate cell division and movement, accelerating tissue repair. Cellular therapies, like stem cell therapy, introduce new cells to the wound bed to promote regeneration. These treatments offer significant hope for patients with non-healing wounds, though continued research is essential to fully understand and utilize their potential.
Hyperbaric Oxygen Therapy: Enhancing Oxygen Delivery
Hyperbaric oxygen therapy (HBOT) involves breathing pure oxygen in a pressurized environment. This increases the amount of oxygen dissolved in the blood, which in turn stimulates blood vessel growth and improves the body's ability to fight infection within the wound. HBOT has shown notable benefits in treating certain types of chronic wounds, such as diabetic foot ulcers with poor blood flow (ischemia). However, specific patient selection criteria are essential for successful treatment.
The Future of Chronic Wound Care: Continued Innovation
The chronic wound care market is constantly evolving. The market is projected to reach approximately $24 billion by 2032, growing at a 7% compound annual growth rate (CAGR). You can explore more detailed statistics here. New technologies, such as 3D-printed skin tissues and advancements in artificial intelligence (AI), are poised to further transform chronic wound care, potentially leading to even more effective and personalized treatments.
Practical Application and Challenges: Addressing Real-World Considerations
While these breakthrough therapies offer exciting advancements, it's crucial to consider practical aspects. Cost-effectiveness, access to specialized equipment and trained healthcare professionals, and appropriate patient selection are all key factors that influence implementation. Continued research is also essential for refining these therapies and developing new strategies. You can also learn more about at-home wound care here. These combined efforts hold great promise for improving patient outcomes and reducing the overall burden of chronic wounds.
Nutrition Strategies That Accelerate Healing From Within
Chronic wound care often prioritizes external treatments. However, the role of nutrition in healing is just as critical. This section explores how specific nutrients influence healing at a cellular level, highlighting the importance of nutritional interventions.
The Cellular Connection: How Nutrients Fuel Healing
Nutrients are essential building blocks for tissue repair and immune system support. Protein, for instance, provides the amino acids required for new cell generation and damaged tissue repair. Consider protein the foundation upon which wound healing is built. Vitamins and minerals act as catalysts in crucial biochemical reactions necessary for the healing process. Vitamin C, in particular, is vital for collagen synthesis, the protein that provides structure and strength to our skin.
Adequate hydration is also fundamental for maintaining cell function and efficient nutrient delivery. Much like a plant needs water to flourish, our cells require proper hydration to function optimally during wound healing. This means appropriate nutrition, including sufficient protein, micronutrients, and hydration, is paramount for supporting the body's inherent healing mechanisms.
Nutritional Screening: Identifying Hidden Deficiencies
Many individuals with chronic wounds experience underlying nutritional deficiencies that can impede healing. Effective wound clinics utilize nutritional screening to uncover these often-overlooked deficiencies. This typically involves assessing a patient’s dietary intake, medical history, and relevant laboratory results. This comprehensive approach helps pinpoint specific nutritional needs and allows for personalized interventions.
Evidence-Based Protocols: Optimizing Nutrient Delivery
Once deficiencies are identified, specific protocols can be implemented to optimize nutrient delivery. These strategies may include:
- Protein Supplementation: For those with low protein intake, supplements can help meet the increased demands of wound healing.
- Micronutrient Delivery: Addressing vitamin and mineral deficiencies with targeted supplements provides the body with the resources needed for effective repair.
- Hydration Management: Implementing strategies to maintain optimal hydration, particularly in patients with fluid restrictions or other medical conditions, is crucial.
These focused interventions can effectively support tissue regeneration and enhance the overall healing process. You might find this resource helpful: How to master choosing the best wound healing supplements.
Real-World Approaches: Addressing Nutritional Challenges
Putting nutritional interventions into practice in real-world scenarios can present obstacles. For example, elderly patients may experience decreased appetite or difficulty swallowing, making it harder to meet their nutritional needs. Patients with limited resources might face challenges accessing healthy foods or affording supplements. However, innovative solutions like meal assistance programs, fortified foods, and partnerships with community organizations can help address these difficulties.
Synergistic Healing: Integrating Nutrition and Topical Treatments
Nutritional therapy works most effectively when integrated with other chronic wound care treatments. For example, combining adequate protein intake with negative pressure wound therapy creates a synergistic effect. The topical treatment encourages wound closure, while proper nutrition provides the necessary components for new tissue growth. This combined approach generally leads to better results than either treatment alone.
By addressing nutritional needs, we empower the body to heal from within. This holistic approach can significantly improve outcomes for chronic wounds, enhancing patients' quality of life and lessening the long-term impact of these challenging conditions.
Digital Revolution in Chronic Wound Care Management

Technology is significantly changing how we approach chronic wound care. From initial assessments to ongoing treatment and monitoring, digital tools are making a real difference. Let's explore some of the key technologies impacting clinical settings today.
AI-Powered Imaging: Bringing Specialist Expertise to Remote Areas
Artificial intelligence (AI) is revolutionizing wound assessment. AI-powered imaging applications, using computer vision, analyze wound images to gather data on wound size, tissue type, and even predict healing potential. This offers a powerful way to extend specialist-level assessments to remote areas with limited access to wound care experts.
This increased access is especially helpful for patients in rural locations or those with mobility challenges. Imagine an AI-powered app analyzing a simple smartphone photo of a wound. This can offer valuable insights that previously required an in-person specialist visit, improving both the speed and accuracy of assessment.
Telehealth in Wound Care: Expanding Access and Reducing Costs
Telehealth expands access to chronic wound care while reducing healthcare costs. Through video consultations and remote monitoring, patients connect with wound care specialists without the need for clinic visits. This offers tremendous benefits for those in underserved communities or with limited mobility.
Telehealth also facilitates more frequent monitoring, which is crucial for early detection of complications. By addressing issues early, interventions can be more effective, potentially preventing wound deterioration and reducing costly hospitalizations.
Smart Dressings and Wearable Sensors: Continuous Monitoring and Early Detection
Smart dressings and wearable sensors provide another advancement in chronic wound care. These devices constantly monitor the wound environment, tracking important factors such as temperature, pH, and moisture levels. This continuous stream of data provides clinicians with valuable insights into the healing process, alerting them to subtle changes before they become visually apparent.
For instance, a change in wound temperature could indicate an infection even before any visible signs appear. This early detection facilitates prompt intervention, improving healing outcomes and preventing potential complications. You can find further information on wound healing in this article: How to master choosing the best foods for wound healing.
Challenges and Solutions in Digital Integration
While digital tools offer clear benefits, integrating them into existing healthcare systems presents some challenges.
-
Technology Accessibility: Not everyone has access to smartphones or reliable internet service, which can limit the reach of some digital tools. However, initiatives to expand broadband access and provide devices are helping to address this gap.
-
Reimbursement Hurdles: Insurance coverage for telehealth services and digital wound care technologies can vary, creating financial barriers. As evidence of the effectiveness and cost-savings of these technologies grows, reimbursement policies are evolving.
-
Data Security and Privacy: Protecting patient data is paramount with any digital health technology. Robust security measures and strict adherence to privacy regulations are essential to build trust and ensure responsible use.
These are just a few examples of how technology is transforming chronic wound care. By tackling the challenges with practical solutions, we can unlock the full potential of digital tools to improve healing outcomes and improve the quality of life for people living with chronic wounds. The field is constantly advancing, promising even more sophisticated and accessible solutions in the future.
Building Wound Care Programs That Actually Work
The success of a chronic wound care program depends on systematic implementation and a commitment to continuous improvement. Much like a well-oiled machine, a thriving program requires coordinated effort across all levels of care. This includes everything from the organizational structure and team dynamics to clinical workflows and performance tracking.
Organizational Structure and Team Composition: The Foundation of Success
Effective chronic wound care programs often use a multidisciplinary approach. This involves a team of specialists from various healthcare fields.
- Physicians: Provide medical oversight and guide treatment plans.
- Nurses: Deliver direct patient care and wound assessments.
- Physical Therapists: Address mobility issues and promote exercise.
- Dietitians: Optimize nutrition for better healing.
- Social Workers: Connect patients with necessary resources and support.
This collaborative model ensures comprehensive care, addressing all aspects of a patient's needs.
Clinical Workflows and Standardized Protocols: Ensuring Consistency
Standardized protocols maintain high-quality care while allowing for individualized treatment. These protocols provide clear guidelines for wound assessment, dressing selection, infection control, and other essentials of chronic wound care. This consistency reduces variability in treatment and leads to better outcomes.
Standardization, however, doesn't mean a rigid approach. Protocols should be flexible, allowing clinicians to adapt treatment plans to each patient's specific needs.
Performance Metrics and Tracking Systems: Driving Continuous Improvement
Tracking key performance indicators (KPIs) provides valuable data for measuring program effectiveness. Metrics like healing rates, infection rates, and patient satisfaction offer insights into areas for improvement. Tracking systems that monitor these KPIs allow for data-driven decisions and continuous quality improvement.
This data-driven approach is essential for identifying trends, evaluating interventions, and making informed adjustments to program protocols. For example, high infection rates may signal a need to review infection control procedures.
Staff Education and Communication Strategies: Fostering Collaboration
Ongoing staff education is crucial for maintaining high clinical competency in chronic wound care. Regular training sessions, workshops, and access to the latest research keep the team informed about best practices and emerging therapies. Effective communication strengthens multidisciplinary collaboration. Regular team meetings, clear communication channels, and shared Electronic Health Records (EHR) facilitate information sharing and care coordination.
To explore technology's role in healthcare, consider the potential of drone management: AI and Automation.
Implementing Realistic Steps for Success
Building a successful chronic wound care program takes time. It requires a step-by-step approach tailored to the specific healthcare setting.
- Needs Assessment: Understanding the patient population's specific needs informs program development.
- Clear Mission and Goals: This creates a shared vision and guides the program's direction.
- Leadership Support: This is crucial for resource allocation and program sustainability.
- Multidisciplinary Team: Assembling a qualified team with expertise in various wound care areas is fundamental.
- Standardized Protocols and Tracking Systems: These ensure consistency and facilitate data-driven decisions.
These steps provide a framework for a program that delivers results. Building a successful chronic wound care program is a continuous process of evaluation, adaptation, and refinement.
For at-home wound care, consider Rapid Wound Care. Their specialized team provides personalized treatment and support for individuals with chronic wounds, aiming to improve healing and overall well-being.

