Understanding Wound Healing and How to Speed It Up
Want to heal wounds faster? This listicle explores eight proven methods to accelerate wound healing and minimize scarring. Whether a minor cut or a chronic wound, discover effective strategies ranging from moist wound healing to advanced therapies like hyperbaric oxygen and growth factors. We'll cover negative pressure wound therapy (NPWT), platelet-rich plasma (PRP), advanced wound dressings, bioengineered skin substitutes, and electrical stimulation. Learn how these methods promote faster healing and improve your overall recovery.
1. Moist Wound Healing
Moist wound healing is a revolutionary approach to wound care that focuses on maintaining a moist environment at the wound site to promote faster and more effective healing. This technique works by preventing cell dehydration, which is crucial for cell migration and the overall regeneration of tissue. Unlike traditional dry wound healing, which allows a scab to form, moist wound healing creates an optimal environment for the body's natural healing processes to accelerate. This method minimizes scab formation, as scabs can actually impede the migration of the epithelial cells necessary for rebuilding healthy tissue.

This approach offers a range of benefits, including creating a balanced moist environment, preventing scab formation that slows healing, facilitating cell migration across the wound, and reducing pain during dressing changes. When proper dressings are used, moist wound healing also decreases the risk of infection. The advantages are clear: studies show up to 50% faster healing times compared to dry healing, reduced scarring for improved cosmetic outcomes, less pain at the wound site, and the convenience of less frequent dressing changes.
While moist wound healing offers significant advantages, it's important to be aware of potential drawbacks. Choosing the correct dressing is crucial, and some specialized dressings can be expensive. Overly moist environments can lead to maceration (excessive softening of the skin), and this method might not be suitable for all wound types. Therefore, proper application and monitoring are essential.
Moist wound healing has become a cornerstone of modern wound care. It's widely used in burn treatment centers globally, has become standard practice in treating diabetic foot ulcers, and is implemented in most modern surgical wound care protocols. The pioneering research of Dr. George Winter in 1962 first demonstrated the benefits of faster epithelialization in moist environments. Today, companies like Johnson & Johnson, Smith & Nephew, and ConvaTec are leading innovators in moist wound healing technologies.
Tips for Effective Moist Wound Healing:
- Choose the right dressing: Select a moisture-retentive dressing appropriate for the specific wound type. Hydrogels, hydrocolloids, and film dressings are common options.
- Cleanse the wound: Ensure the wound is thoroughly cleaned before applying any dressing.
- Follow instructions: Adhere to the manufacturer's guidelines for dressing changes.
- Monitor regularly: Keep a close eye on the wound for any signs of maceration or infection.
Moist wound healing deserves its place on this list because it represents a significant advancement in wound care, offering a faster, less painful, and more aesthetically pleasing path to recovery. Learn more about Moist Wound Healing to discover how this method can help heal wounds faster and more effectively. Whether you're a patient managing a chronic wound, a caregiver, or a healthcare professional, understanding the principles of moist wound healing can greatly improve patient outcomes.
2. Negative Pressure Wound Therapy (NPWT)
Negative Pressure Wound Therapy (NPWT), also known as vacuum-assisted closure (VAC), is an advanced wound healing technique that offers a significant advantage in helping wounds heal faster. It uses controlled negative pressure to draw out fluid and infectious materials from the wound bed, creating an optimal environment for healing. This system typically consists of a specialized dressing sealed over the wound, connected by tubing to a vacuum pump. The pump creates gentle suction, removing excess fluid and promoting the growth of healthy granulation tissue. This therapy helps accelerate healing by reducing swelling (edema), increasing local blood flow and oxygenation, removing exudate (drainage), and stimulating the formation of new tissue.

NPWT boasts several key features contributing to its effectiveness: the application of controlled negative pressure, removal of excess fluid and exudate, reduction of edema in surrounding tissues, increased local blood flow and oxygenation, promotion of granulation tissue formation, and the creation of a closed, moist wound healing environment. These features work synergistically to expedite the healing process, particularly for complex or challenging wounds.
When and Why to Use NPWT:
NPWT is particularly beneficial for wounds that are struggling to heal using conventional methods. This includes chronic wounds like diabetic foot ulcers and pressure ulcers, as well as acute wounds such as surgical wounds with complications or traumatic injuries. It is often a preferred method for deep wounds, heavily draining wounds, and wounds with a high risk of infection. By creating a negative pressure environment, NPWT helps to draw the wound edges together, reduce swelling, and promote the formation of healthy new tissue.
Examples of Successful Implementation:
NPWT has become a standard of care for many diabetic foot ulcers and is frequently used in treating pressure ulcers in long-term care facilities. It's also applied in managing surgical wounds experiencing complications and has been widely implemented in treating combat injuries in military medicine. Its versatility and effectiveness have made it a valuable tool across various healthcare settings.
Pros and Cons of NPWT:
While highly effective, NPWT does have some considerations.
Pros:
- Effective for complex, deep, or challenging wounds
- Reduces healing time for many wound types
- Decreases frequency of dressing changes
- Can be used in both inpatient and outpatient settings
- Helps manage heavily exuding wounds
Cons:
- Requires specialized equipment and training
- Can be costly
- May cause pain during therapy or dressing changes
- Not suitable for wounds with malignancy, untreated osteomyelitis, or exposed vessels
Tips for Effective NPWT:
- Ensure the wound is thoroughly cleaned before applying NPWT.
- Select appropriate pressure settings based on the wound type and patient comfort.
- Monitor for pain, which may indicate a need to adjust pressure settings.
- Change the dressing every 48-72 hours, or according to protocol.
- Assess the wound regularly for healing progress and complications.
NPWT’s ability to significantly accelerate wound healing, particularly in complex cases, earns it a prominent place on this list. Its unique mechanism of action addresses multiple factors hindering wound healing, making it a valuable tool for both patients and healthcare professionals seeking effective solutions to heal wounds faster. Developed by Dr. Louis Argenta and Dr. Michael Morykwas in the 1990s and popularized by companies like KCI (Kinetic Concepts, Inc.) with their V.A.C. therapy system, along with Smith & Nephew and Mölnlycke Health Care, NPWT has revolutionized wound care and continues to be refined and improved.
3. Platelet-Rich Plasma (PRP) Therapy
Platelet-Rich Plasma (PRP) therapy offers a cutting-edge approach to heal wounds faster. This innovative treatment harnesses the body's natural healing power by concentrating platelets, which are rich in growth factors, and applying them directly to the wound site. Platelets play a crucial role in clotting blood and initiating the healing process. By concentrating them to 5-10 times their normal levels, PRP therapy delivers a potent dose of bioactive proteins that stimulate cell proliferation, collagen synthesis, and tissue regeneration. This autologous therapy – meaning it utilizes the patient's own blood components – minimizes the risk of rejection or allergic reactions, making it a safe and effective option for various wound types.

PRP therapy deserves its place on this list due to its remarkable ability to accelerate healing in chronic non-healing wounds, including diabetic foot ulcers, pressure ulcers, and tendon injuries. Studies have shown significant improvements in healing rates, with some reporting a 70% improvement in diabetic foot ulcer healing. It also offers potential pain reduction and may reduce the need for more invasive surgical procedures. The benefits extend to various fields, from sports medicine (treating tendon and ligament injuries in athletes) to dental surgery (enhancing bone grafting) and wound care for spinal cord injury patients.
How PRP Therapy Works: The process involves drawing a small amount of the patient's blood, similar to a routine blood test. The blood is then processed in a centrifuge to separate the platelet-rich plasma from the other blood components. This concentrated PRP is then carefully applied to the wound area. The concentrated growth factors within the PRP stimulate stem cell migration to the injury site, promote angiogenesis (new blood vessel formation), and accelerate the overall healing cascade.
Benefits of PRP Therapy:
- Accelerated Healing: PRP significantly speeds up the healing process, particularly in chronic wounds that have been resistant to other treatments.
- Reduced Pain: Many patients experience a reduction in pain levels following PRP treatments.
- Minimal Side Effects: Because it uses the patient's own blood, the risk of rejection or allergic reactions is minimal.
- Versatile Application: PRP therapy can be used to treat a variety of wounds and injuries.
Potential Drawbacks:
- Cost: PRP therapy is relatively expensive and is often not covered by insurance.
- Variability: Results can vary significantly between patients.
- Multiple Treatments: Optimal results typically require multiple treatments spaced several weeks apart.
Tips for Patients Considering PRP Therapy:
- Consult a Specialist: Discuss your wound and overall health with a qualified healthcare professional to determine if PRP therapy is right for you.
- Treatment Schedule: Best results are usually achieved with 2-3 treatments spaced 4-6 weeks apart.
- Medication Management: Avoid anti-inflammatory medications before and after treatment as they can interfere with the healing process.
- Hydration: Stay hydrated before the procedure.
- Post-Treatment Care: Carefully follow your healthcare provider's post-treatment instructions.
PRP therapy represents a significant advancement in wound care, offering a powerful tool to heal wounds faster and improve patient outcomes. While it's not a universal solution and does have some limitations, its potential benefits, particularly for challenging wounds, make it a valuable option worth considering.
4. Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric Oxygen Therapy (HBOT) is a specialized medical treatment that can significantly accelerate the healing process of certain types of wounds. It involves breathing 100% pure oxygen within a pressurized chamber, typically at pressures 2-3 times higher than normal atmospheric pressure. This environment supersaturates the blood with oxygen, allowing it to penetrate deep into tissues, even those with compromised blood flow due to injury or disease. The elevated oxygen levels stimulate a cascade of beneficial effects, including the release of growth factors, enhanced white blood cell activity, and the promotion of new blood vessel formation (angiogenesis), all crucial for efficient wound healing. HBOT helps to heal wounds faster by essentially flooding the injured area with the vital element needed for tissue repair and regeneration.
HBOT sessions generally last between 90 and 120 minutes, and multiple sessions are often required to achieve optimal results, often ranging from 20-40 treatments depending on the specific condition. The increased oxygen concentration within the body can be up to 10-15 times higher than normal levels, which is particularly helpful for areas with poor circulation. This boost in oxygen not only aids in tissue repair but also reduces edema through vasoconstriction while simultaneously increasing oxygen delivery. Furthermore, it enhances the antimicrobial activity of white blood cells, making it a powerful tool against certain infections. HBOT also promotes the production of collagen, the essential protein for building and strengthening new tissue.
When and Why to Use HBOT: HBOT isn't a first-line treatment for every wound. It is typically reserved for specific, complex, and non-healing wounds that haven't responded to conventional treatments. It's a recognized and effective treatment for conditions such as diabetic foot ulcers, radiation injuries (often a side effect of cancer treatment), and certain types of infections, particularly anaerobic infections where oxygen is toxic to the causative bacteria. HBOT has been shown to help salvage compromised tissue and skin flaps, making it a valuable asset in reconstructive surgery.
Examples of Successful Implementation: HBOT has demonstrated remarkable success in various clinical settings. Studies involving radiation-induced wounds have shown up to 80% improvement with HBOT. In the management of diabetic foot ulcers, some centers have reported a 40% reduction in amputation rates through the integration of HBOT. Its use in crush injuries and for compromised skin grafts has also yielded positive outcomes, and it's proven effective in managing certain necrotizing soft tissue infections where rapid intervention is crucial.
Pros and Cons: While HBOT offers significant benefits, it’s important to be aware of both its advantages and disadvantages.
Pros:
- Effective for complex, non-healing wounds.
- Approved treatment for specific conditions (e.g., diabetic foot ulcers, radiation injuries).
- Combats certain anaerobic infections.
- Can salvage compromised tissue.
- Non-invasive.
Cons:
- Expensive and time-consuming.
- Limited availability.
- Not suitable for all patients (e.g., certain lung conditions).
- Potential side effects (e.g., ear/sinus barotrauma, temporary myopia).
- Requires specialized facilities and trained personnel.
Tips for Patients Undergoing HBOT:
- Ear Pressure: Clear your ears frequently during the compression and decompression phases of the treatment to avoid discomfort or barotrauma.
- Smoking: Avoid smoking before and after treatments, as it constricts blood vessels and reduces the benefits of HBOT.
- Clothing: Wear 100% cotton clothing during treatments to reduce fire risk due to the high oxygen environment.
- Skin Products: Avoid using petroleum-based products before treatment, as these can be flammable in the high-oxygen environment.
- Standard Wound Care: Combine HBOT with appropriate standard wound care practices for optimal healing outcomes.
HBOT's unique ability to dramatically increase tissue oxygen levels makes it a powerful tool in wound healing. It deserves its place on this list because it provides a viable solution for complex and chronic wounds that often fail to respond to other therapies, ultimately improving patients' quality of life and reducing the risk of serious complications like amputation. While cost and accessibility can be barriers, the potential benefits for appropriate candidates are substantial. For patients with persistent non-healing wounds, discussing HBOT with a wound care specialist is highly recommended.
5. Advanced Wound Dressings: Accelerate Healing and Minimize Complications
Want to heal wounds faster? Advanced wound dressings offer a significant advantage over traditional gauze and can dramatically improve healing outcomes. These specialized dressings are designed to create an optimal environment for wound healing, addressing specific wound types and stages to promote faster recovery and minimize discomfort. They go beyond simply covering the wound; they actively interact with the wound bed to accelerate the body's natural healing processes. This makes them a crucial tool for anyone dealing with chronic or acute wounds.
Unlike basic bandages, advanced wound dressings work by interacting with the wound environment to maintain a delicate moisture balance. This moist wound healing approach is crucial as it promotes cell growth and tissue regeneration. Moreover, these dressings protect against infection, absorb excess fluid (exudate), and can even deliver therapeutic agents directly to the wound site. This targeted approach can significantly reduce healing time compared to conventional dressings.
For example, hydrocolloid dressings have been shown to reduce healing time for pressure ulcers by up to 40%. Similarly, silver-containing dressings are highly effective in burn care, significantly lowering infection rates. For highly exuding wounds like diabetic foot ulcers, foam dressings are an excellent choice. And in surgical wound care, hydrofibers can promote faster healing and minimize scarring. These examples highlight the versatility and effectiveness of advanced wound dressings in diverse clinical settings.
Benefits of Advanced Wound Dressings:
- Optimized Healing: Create the ideal environment for specific wound types and exudate levels.
- Reduced Pain: Minimize discomfort during dressing changes thanks to their non-adherent properties.
- Faster Healing: Accelerate healing compared to traditional gauze.
- Infection Control: Many contain antimicrobial properties to combat infection.
- Targeted Therapy: Some dressings can deliver growth factors or other therapeutic agents.
- Less Frequent Changes: Reduce the frequency of dressing changes, saving time and resources.
Potential Drawbacks:
- Higher Upfront Cost: Advanced wound dressings typically have a higher initial cost than traditional gauze. However, the reduced healing time and potential for preventing complications often lead to lower overall treatment costs.
- Proper Selection Critical: Choosing the correct dressing is vital. It requires assessment of the wound type, location, and exudate level.
- Potential for Allergies: Some patients might be allergic to certain components of advanced dressings.
- Specific Storage: Certain dressings may have specific storage requirements.
- Application Training: Some advanced dressings might require specialized training for proper application.
Actionable Tips for Using Advanced Wound Dressings:
- Accurate Assessment: Select the appropriate dressing based on wound type, location, and the amount of exudate.
- Cleanliness is Key: Thoroughly clean the wound before applying a new dressing.
- Follow Instructions: Adhere to the manufacturer's guidelines for wear time and changing frequency.
- Monitor for Changes: Be vigilant for signs that indicate a dressing change is needed, such as leakage or increased pain.
- Cost-Effectiveness: Consider the overall cost-effectiveness, factoring in healing time and potential complications, rather than just the unit price.
Learn more about Advanced Wound Dressings
Companies like ConvaTec, Smith & Nephew, 3M Healthcare, and Mölnlycke Health Care have been instrumental in developing and popularizing these innovative wound care solutions. The concept of moist wound healing, pioneered by Dr. T.D. Turner, has revolutionized wound care and laid the foundation for these advanced products.
Advanced wound dressings deserve a place on this list because they represent a significant advancement in wound care, offering faster healing, reduced pain, and a lower risk of complications. By creating an optimal healing environment, these dressings empower patients and healthcare providers to achieve better wound healing outcomes. They are particularly beneficial for patients with chronic wounds or those at high risk for complications, contributing significantly to improved quality of life.
6. Growth Factor Therapy: Accelerate Healing at the Cellular Level
If you're looking to heal wounds faster, particularly chronic ones that refuse to budge, growth factor therapy might be a game-changer. This innovative approach harnesses the power of naturally occurring proteins to supercharge your body's healing mechanisms. It deserves a spot on this list due to its targeted action and potential for significant healing improvements, especially for complex wounds.
Growth factor therapy works by applying concentrated bioactive proteins directly to the wound site. These proteins, which are crucial regulators of cell division, migration, and protein synthesis, essentially give your body's natural healing process a boost. By augmenting the levels of these factors, the therapy can jump-start stalled healing and encourage faster tissue regeneration. This targeted approach addresses specific phases of the wound healing cascade, from initial inflammation control to the final stages of tissue remodeling, making it a powerful tool to heal wounds faster.
How Growth Factors Help Heal Wounds Faster:
Growth factors are like messengers that tell cells what to do. Different types of growth factors target specific aspects of wound healing:
- Stimulating cell growth and division: This helps rebuild damaged tissue.
- Promoting blood vessel formation (angiogenesis): This ensures adequate blood supply to the wound for nutrient delivery and waste removal.
- Attracting cells involved in repair: This coordinates the body's healing response.
- Reducing inflammation: This creates a more optimal healing environment.
Examples of Growth Factor Therapy in Action:
- Becaplermin (Regranex) gel: This FDA-approved treatment, containing platelet-derived growth factor (PDGF), is used for diabetic foot ulcers and has shown up to a 43% improvement in complete wound closure.
- Epidermal Growth Factor (EGF) treatment: Often used in burn care to stimulate skin regeneration.
- Platelet-Derived Growth Factor therapy: Beneficial in the management of pressure ulcers.
- Recombinant human growth factors: Utilized in various surgical wound complications.
Pros and Cons of Growth Factor Therapy:
Pros:
- Effective for chronic wounds: Offers a solution when conventional treatments fail.
- Significantly reduces healing time: Accelerates the natural healing process.
- Targeted healing: Addresses specific deficiencies in the wound healing cascade.
- Minimal systemic effects (topical application): Reduces the risk of side effects compared to systemic treatments.
- Some formulations available for at-home application: Offers convenience and potentially reduces healthcare visits.
Cons:
- Expensive: Can be significantly more costly than traditional wound care.
- Variable response rates: Effectiveness can differ between individuals.
- Theoretical cancer risk: Although clinical evidence is limited, there's a theoretical concern about promoting cancerous growth. Discuss this with your doctor.
- Careful storage and handling: Many growth factors are temperature-sensitive.
- Multiple applications may be necessary: Complete healing might require repeated treatments.
Actionable Tips for Using Growth Factor Therapy:
- Cleanliness is key: Ensure the wound is thoroughly cleaned before each application.
- Follow storage guidelines: Maintain the product's efficacy by adhering to storage instructions.
- Precise application: Use the exact amount prescribed. More is not necessarily better.
- Continue basic wound care: Growth factor therapy complements, but doesn't replace, standard wound care practices.
- Monitor progress: Track healing by taking regular photographs of the wound.
When and Why to Consider Growth Factor Therapy:
Growth factor therapy is typically considered when wounds fail to heal with conventional treatments. It's especially beneficial for chronic wounds like:
- Diabetic foot ulcers
- Pressure ulcers
- Venous leg ulcers
- Non-healing surgical wounds
- Burns
If you're struggling with a wound that just won't heal, talk to your doctor about whether growth factor therapy might be right for you. It could be the key to finally achieving complete wound closure and healing wounds faster.
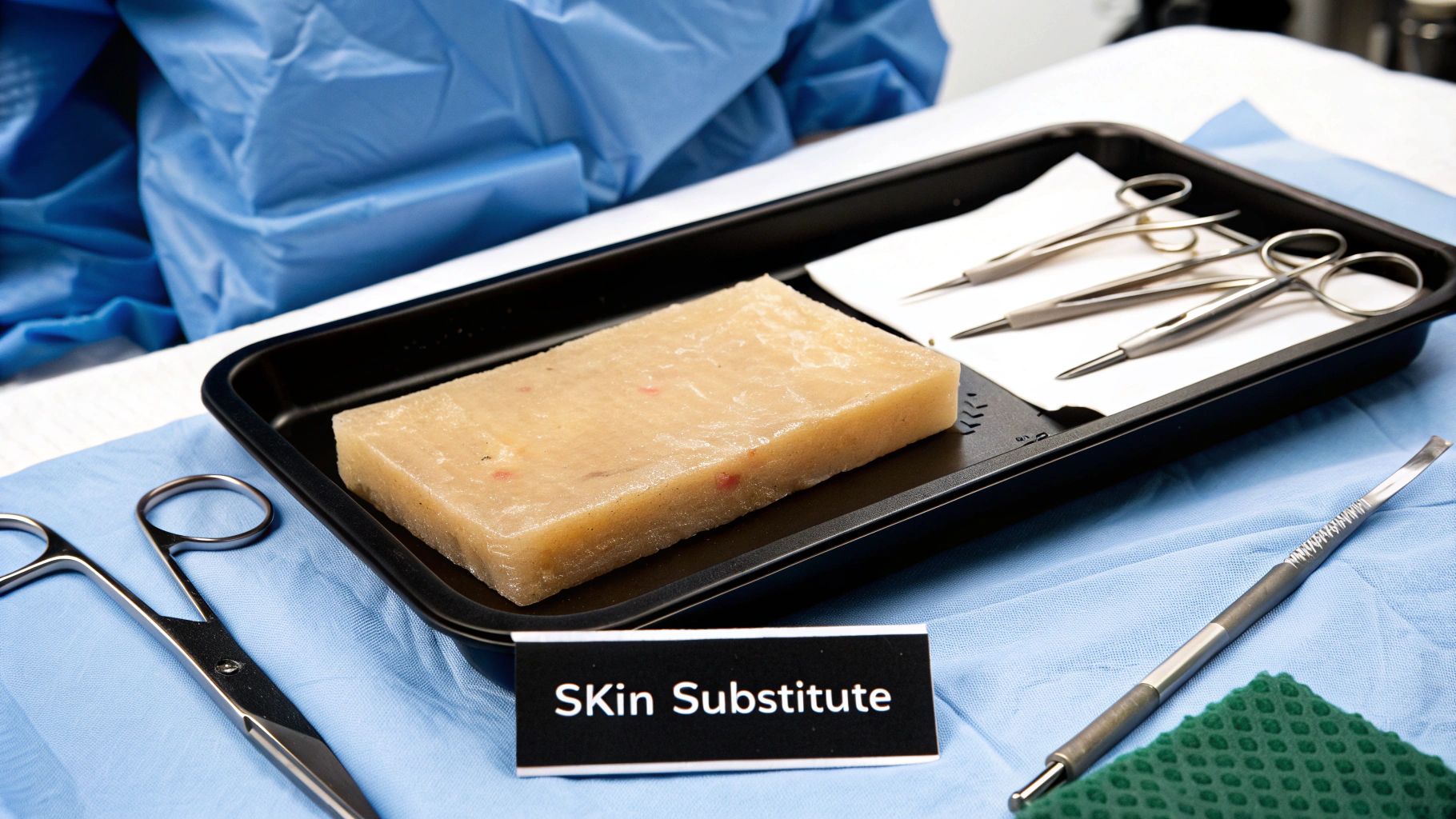
7. Bioengineered Skin Substitutes: Accelerating Wound Healing
If you're looking to heal wounds faster, especially large, complex, or chronic ones, bioengineered skin substitutes may offer a significant advantage. These advanced wound care products act as temporary or permanent replacements for damaged skin, actively promoting healing and reducing recovery time. They work by providing a scaffold for new tissue growth, delivering growth factors, and protecting the wound from further damage while the body's natural healing processes take over. This makes them a powerful tool in the fight against slow-healing wounds.
Bioengineered skin substitutes range from simple collagen matrices to complex living skin equivalents. Some are acellular, derived from natural tissues, while others are cellular, containing living human cells like fibroblasts and keratinocytes. They can even be made of synthetic materials. These substitutes are available in various forms, including sheets, gels, sprays, and injectables, allowing for tailored application based on the specific wound. Some even incorporate both dermal and epidermal components for a more complete skin replacement.
How They Help Heal Wounds Faster:
Bioengineered skin substitutes provide several key benefits that contribute to faster healing:
- Structural Support: They act as a framework for new cells and blood vessels to grow into, accelerating tissue regeneration.
- Growth Factor Delivery: Some substitutes release growth factors and cytokines, which stimulate cell proliferation and migration, further speeding up the healing process.
- Protection: They shield the wound from external contaminants and trauma, reducing the risk of infection and promoting a more optimal healing environment.
When to Consider Bioengineered Skin Substitutes:
These advanced wound care products are particularly valuable in the following situations:
- Large Wounds: For wounds with substantial tissue loss, where natural healing is slow and challenging.
- Burns: In the treatment of severe burns, where skin regeneration is significantly compromised.
- Chronic Ulcers: For chronic wounds like diabetic foot ulcers or venous leg ulcers, which often struggle to heal on their own.
Examples of Successful Implementation:
Several bioengineered skin substitutes have demonstrated remarkable success in healing wounds faster:
- Apligraf: A living bi-layered skin substitute that has shown twice the healing rate for venous leg ulcers compared to standard care.
- Integra Dermal Regeneration Template: Widely used in severe burn treatment to promote skin regeneration and reduce scarring.
- AlloDerm: Utilized in reconstructive surgery and complex wound healing to provide structural support and facilitate tissue integration.
- Dermagraft: Employed in diabetic foot ulcer treatment, demonstrating a 30% improvement in healing rates.
Tips for Optimal Use:
To maximize the benefits of bioengineered skin substitutes:
- Wound Bed Preparation: Thoroughly clean and debride the wound bed to remove any necrotic tissue before application.
- Adherence to Protocols: Strictly follow the product-specific application and care instructions provided by the manufacturer.
- Monitoring: Regularly monitor the wound for signs of infection or graft rejection.
- Secondary Dressings: Use appropriate secondary dressings as recommended to protect the substitute and maintain a moist wound environment.
- Follow-up: Schedule follow-up assessments with your healthcare provider at the recommended intervals.
Pros and Cons:
While highly effective, bioengineered skin substitutes come with certain considerations:
Pros:
- Effective for large and chronic wounds
- Dramatically reduces healing time
- Reduces pain and dressing changes
- May improve scarring and functional outcomes
- Some can be used in infected wounds
Cons:
- Expensive compared to conventional treatments
- May require specialized storage (refrigeration)
- Limited shelf life for cellular products
- May require multiple applications
- Variable integration rates
Why They Deserve a Place on This List:
Bioengineered skin substitutes represent a significant advancement in wound care, offering a faster and more effective way to heal challenging wounds. Their ability to actively promote tissue regeneration, reduce healing time, and improve patient outcomes makes them a valuable tool for both patients and healthcare professionals. They are a crucial option to consider when traditional wound care methods fall short.
While no website link is readily available for a comprehensive overview of all bioengineered skin substitutes, researching the specific products mentioned above (Apligraf, Integra, AlloDerm, Dermagraft) will provide more detailed information.
8. Electrical Stimulation Therapy
Want to heal wounds faster? Electrical Stimulation Therapy (EST) may be a viable option. This innovative therapy utilizes controlled electrical currents to jumpstart the body's natural healing process, helping wounds mend more efficiently. It mimics the body's own bioelectrical system, which generates electrical signals in response to skin damage. By applying specific types of electrical currents to the wounded tissue, EST can increase circulation, enhance cell migration (the movement of cells to the wound site for repair), stimulate tissue granulation (the formation of new connective tissue and blood vessels), reduce swelling (edema), and may even offer antibacterial effects.
EST works by delivering low-level electrical currents to the wound tissue using various waveforms (continuous, pulsed, alternating) and electrode placements (direct or indirect contact with the wound). The current strength, typically ranging from microamperes to milliamperes, along with other adjustable parameters like pulse duration and frequency, can be tailored to the specific wound type, the phase of healing, and individual patient characteristics. Sessions usually last between 20-60 minutes. Different parameters target specific healing phases, ensuring optimal therapeutic benefit throughout the healing journey. For example, a positive current (anode) is often used for infected wounds, while a negative current (cathode) promotes tissue stimulation.
This method has shown remarkable results in diverse healthcare settings. Veterans Affairs hospitals have successfully implemented EST for chronic pressure ulcers, demonstrating up to a 50% improvement in healing rates. Outpatient clinics utilize it for diabetic foot ulcers, and it's even applied in sports medicine for acute injury management. EST is also integrated into comprehensive care plans for venous leg ulcers. These real-world applications highlight the versatility and potential of this therapy across various wound types.
Why choose EST?
- Non-invasive and generally painless: Most patients experience minimal discomfort during treatment.
- Effective for stalled wounds: It can reignite the healing process in chronic wounds that have stopped responding to other treatments.
- Improved circulation and oxygenation: EST promotes blood flow and increases oxygen delivery to the wound bed, essential for tissue repair.
- Potential antibacterial effects: Some studies suggest EST can inhibit bacterial growth, reducing infection risk.
- Versatile treatment option: It can be used in conjunction with other wound care therapies, like dressings and compression therapy.
- Home use options: Portable EST units are available, allowing patients to continue treatment at home.
Considerations:
- Requires specialized equipment and training: Healthcare professionals must be properly trained to administer EST effectively and safely.
- Effectiveness depends on proper parameter selection: Accurate assessment and individualized treatment plans are crucial.
- Multiple sessions needed: Consistent treatment, typically 3-5 times per week, is necessary for optimal results.
- Contraindications: EST is not suitable for patients with electronic implants (e.g., pacemakers), malignancies near the wound site, or certain metallic materials in the wound area.
- Insurance coverage: Reimbursement policies for EST vary, so checking your insurance coverage beforehand is advisable.
Tips for optimizing EST:
- Wound preparation: Ensure the wound is thoroughly cleaned and debrided (removal of dead tissue) before treatment.
- Gradual intensity increase: Begin with lower current intensities and gradually adjust upwards based on patient tolerance.
- Documentation: Carefully document wound characteristics before starting therapy to monitor progress effectively.
- Moisture retention: Use appropriate moisture-retentive dressings between treatments to support the healing process.
Learn more about Electrical Stimulation Therapy
Pioneering figures like Dr. Luther C. Kloth and Dr. Mary Dyson, who conducted groundbreaking studies in the 1980s, have paved the way for the widespread adoption of EST. Companies like MIST Therapy Systems and Prizm Medical, Inc., have developed advanced EST devices, and the Center for Medicare Services' acceptance of EST as a reimbursable therapy for certain wounds further validates its importance in modern wound care. For patients with chronic or acute wounds, primary care providers, long-term care facilities, wound care specialists, and even Medicare beneficiaries, especially elderly patients, exploring the possibility of EST can be a crucial step toward faster and more efficient healing.
8 Techniques for Faster Wound Healing Comparison
| Technique | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Moist Wound Healing | Moderate: Requires proper dressing selection and monitoring | Moderate: Specialized dressings needed, some costly | Faster healing (up to 50%), reduced scarring and pain | Burns, diabetic foot ulcers, surgical wounds | Accelerates healing, less pain, fewer dressing changes |
| Negative Pressure Wound Therapy (NPWT) | High: Needs specialized equipment and trained staff | High: Vacuum pump, dressings, consumables | Accelerated healing, edema reduction, granulation tissue growth | Complex, deep, or heavily exuding wounds, inpatient/outpatient | Effective in challenging wounds, reduces dressing frequency |
| Platelet-Rich Plasma (PRP) Therapy | High: Requires blood draw, processing equipment, skilled personnel | High: Centrifuge, kits, multiple sessions often needed | Enhanced healing in chronic wounds, tissue regeneration | Chronic non-healing wounds, sports injuries, dental surgeries | Autologous, minimal rejection, stimulates angiogenesis |
| Hyperbaric Oxygen Therapy (HBOT) | Very High: Specialized pressurized chambers and trained operators | Very High: Chamber facilities with time-intensive sessions | Increases oxygen delivery, promotes angiogenesis and immune response | Diabetic wounds, radiation injuries, crush injuries, infections | Non-invasive, improves tissue oxygenation, combats anaerobic infection |
| Advanced Wound Dressings | Moderate: Proper assessment and selection necessary | Moderate: Various specialized dressings, may need training | Reduced healing time, infection control, moisture balance | Pressure ulcers, burns, diabetic foot ulcers | Interactive, antimicrobial options, less frequent changes |
| Growth Factor Therapy | High: Requires controlled application and storage | High: Recombinant proteins, storage requirements | Faster healing in chronic wounds, targets healing phases | Chronic wounds unresponsive to other treatments | Targets specific healing deficits, minimal systemic effects |
| Bioengineered Skin Substitutes | Very High: Complex products needing specialized handling | Very High: Expensive, storage sensitive, multiple applications | Dramatic healing acceleration in large or chronic wounds | Large tissue loss, burns, chronic ulcers | Structural support, growth factor delivery, reduces scarring |
| Electrical Stimulation Therapy | High: Requires device, trained personnel, multiple sessions | Moderate to High: Equipment needed, multiple treatments | Improves blood flow, restarts stalled healing | Chronic wounds, pressure ulcers, diabetic foot ulcers | Non-invasive, antibacterial effects, portable for home use |
Choosing the Right Wound Care Approach for Faster Healing
Effectively healing wounds faster isn't a one-size-fits-all process. This article explored a range of approaches, from fundamental practices like moist wound healing and utilizing advanced wound dressings, to more specialized therapies such as Negative Pressure Wound Therapy (NPWT), Platelet-Rich Plasma (PRP), Hyperbaric Oxygen Therapy (HBOT), Growth Factor Therapy, Bioengineered Skin Substitutes, and Electrical Stimulation Therapy. The optimal strategy depends on several key factors: the nature and severity of your wound, your overall health, and the resources available to you. While some techniques can be integrated into at-home care, others necessitate specialized equipment and the guidance of healthcare professionals.
Mastering these concepts empowers you to take an active role in your healing journey. For further insights into accelerating the healing process, explore this comprehensive guide on how to speed up wound healing from PEPTYS, which offers valuable perspectives on tissue regeneration. By understanding the various options and collaborating with your healthcare team, you can significantly influence the speed and effectiveness of your recovery, ultimately improving your quality of life and overall well-being. Remember, healing is a journey, not a race, and taking informed steps towards recovery is the most crucial action you can take.
Are you ready to take control of your wound healing and experience faster, more effective results? Rapid Wound Care specializes in personalized wound care plans designed to optimize healing based on your unique needs. Visit Rapid Wound Care today to learn how they can help you achieve a swift and complete recovery.

